Mood disorders and mental illness are common manifestations of Lyme disease and other tick-borne infections. In acute Lyme disease, cognitive impairment (what most refer to as brain fog) is a common symptom. However, when tick-borne infections go undiagnosed for a long period of time, people can experience a range of neuropsychiatric symptoms. Lyme disease can cause anxiety, panic attacks, depression, bipolar disorder, developmental disorders, autism, schizophrenia, PTSD, addiction, insomnia, cognitive impairment, dementia, violence, and even suicide.

There are over 400 peer-reviewed articles discussing the association between Lyme disease and neuropsychiatric symptoms. The biggest challenge for people suffering from mood disorders is most mental health practitioners are not trained to look for the underlying cause(s) of the symptoms – including Lyme disease. Many people end up on mood-stabilizing medication for years – or a lifetime – without a known cause of their symptoms. In some with Lyme disease, mood symptoms may improve on psychotropic medication, but symptoms often relapse.
If a mood disorder is caused by Lyme disease or an associated infection, it may present as “atypical.” This is because the symptoms do not have the usual characteristics of the mood disorder while also having additional symptoms such as fatigue, joint pain, or headaches.
What Causes Neuropsychiatric Symptoms in Lyme Disease?
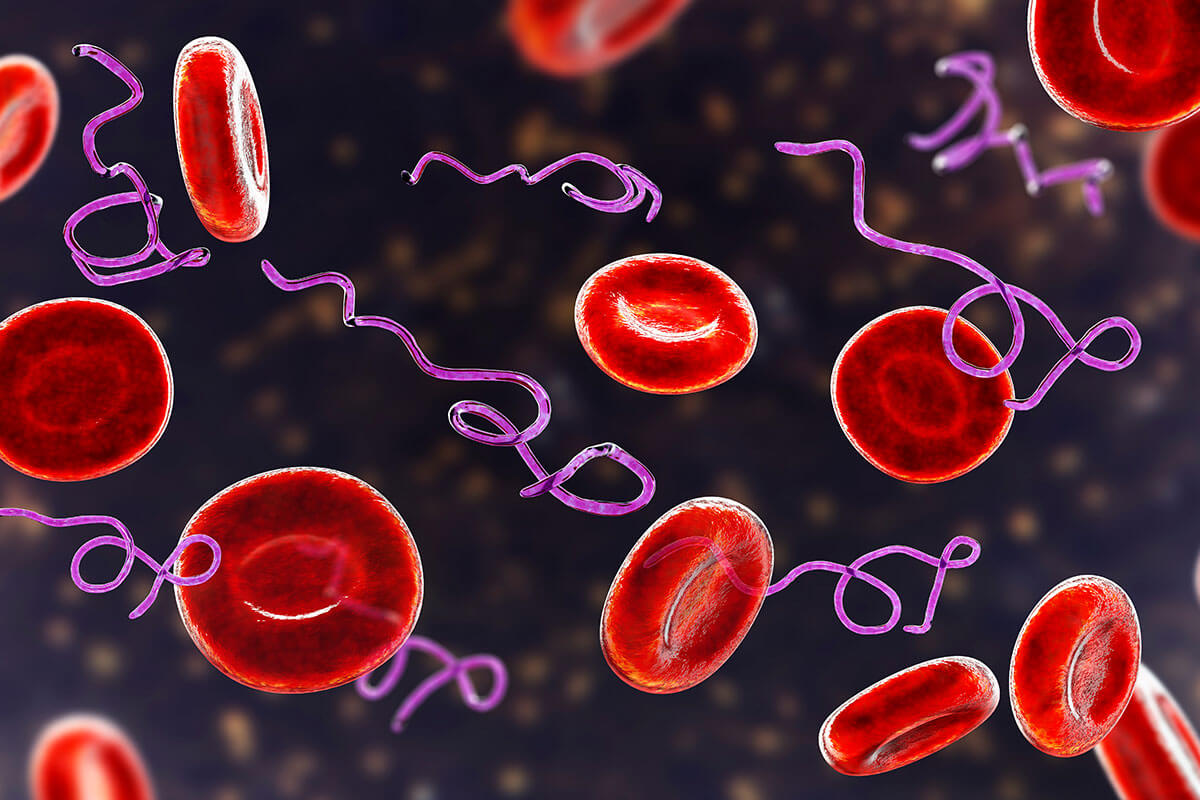
In tick-borne infections, it is believed damage to the nervous system can occur in three ways leading to neuropsychiatric symptoms. In the vascular form, tissue death in the brain can take place. In addition, infection with Borrelia within the central nervous system can lead to atrophy and encephalitis of the brain. The third type of damage happens outside of the central nervous system and causes an inflammatory response that affects the central nervous system.
Like many systemic symptoms associated with Lyme disease, neuropsychiatric symptoms can be caused by the immune response sparking inflammation.
The persistent immune response – even after the pathogen has been eliminated – includes inflammatory cytokines and autoimmune processes. Lyme bacteria has been shown to trigger antibodies to neuronal tissue leading to neurodegeneration.
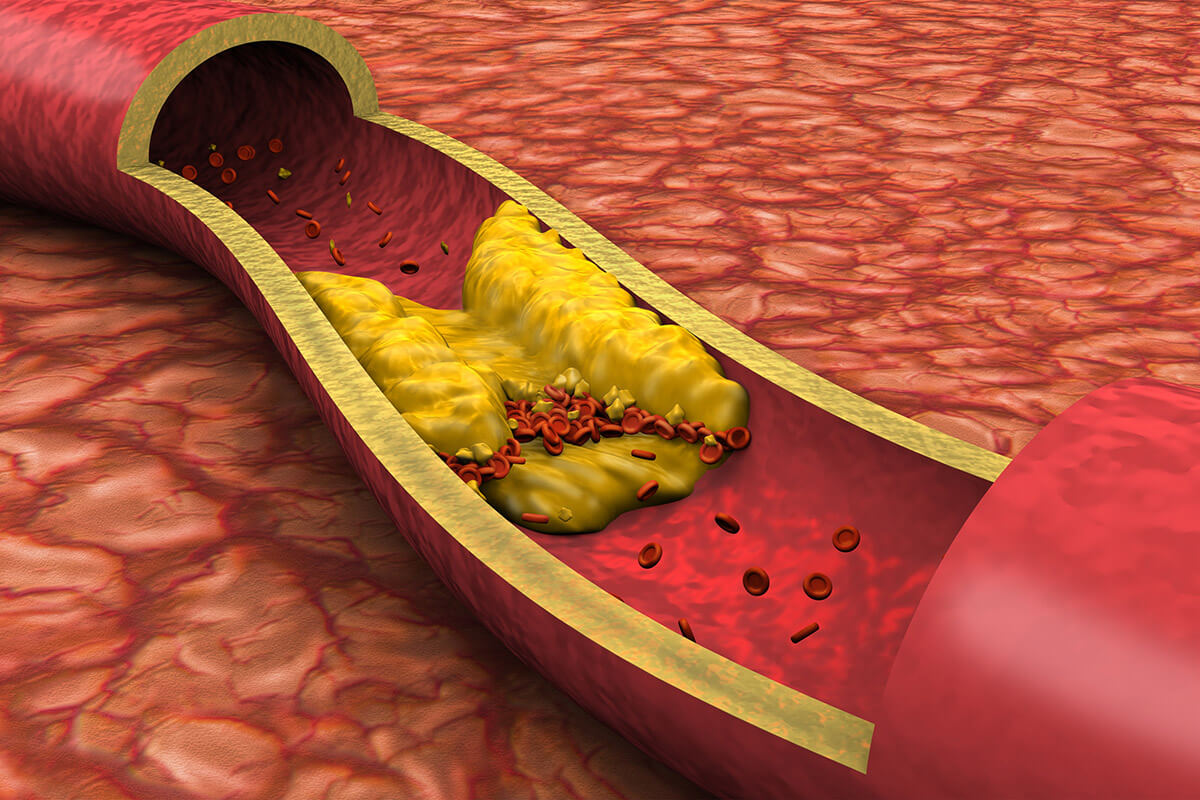
Metabolic changes can also be induced by Lyme infections. The mitochondria in the central nervous system can become damaged from oxidative stress associated with tick-borne infections. Mitochondrial dysfunction leads to cognitive issues and fatigue. Inflammatory cytokines also cause an increase in quinolinic acid, a metabolite that contributes to neurotoxicity. People infected with Lyme borreliosis have increased levels of quinolinic acid in their central nervous system contributing to depression and poor cognition.
Imaging studies in people with Lyme disease often demonstrate pathophysiological changes of the brain that are not typically seen in depression. SPECT scans will illustrate decreased blood flow to the frontal and temporal lobes in Lyme disease. Swelling and atrophy in different regions of the brain can be seen on NeuroQuant MRI, which is consistent with an infectious or inflammatory cause of a mood disorder.
Lyme Disease and Depression
When properly treated following an acute infection with Lyme disease, depression rarely manifests.
In patients who are not properly diagnosed or effectively treated and end up with late-stage Lyme disease, depression is common. People suffering from depression caused by tick-borne infections will also often experience other symptoms such as fatigue, headaches, and/or joint pain. These additional symptoms are a good indication there may be a systemic illness causing the depression.
Since it can take years for a proper diagnosis of late-stage Lyme disease, it is common for people suffering from depression to be prescribed antidepressants. They often have to try multiple antidepressants because their depression was not alleviated by the initial medications. It may be important to remain on an antidepressant even after a diagnosis of Lyme disease is made to help stabilize one’s mood. Typically after effective treatment of late-stage Lyme disease, people are able to wean off of their psychotropic medications.
Major depressive disorder can be associated with underlying medical conditions such as tick-borne infections. Symptoms of major depressive disorder may include depressed mood, irritability, mood swings, insomnia, fatigue, poor concentration, and cognitive issues.
In addition to the physiological changes that occur in Lyme disease, being sick with a chronic illness can cause depression from not being able to perform daily activities, enjoy hobbies, engage in relationships, or from living with the uncertainty of a chronic medical condition.
Aaron suffered from panic attacks, depression, and insomnia. He was referred to me by his psychiatrist to be evaluated for tick-borne infections because the presentation of his symptoms were atypical. Aaron also complained of migraines, fatigue, and difficulty concentrating. He had not been in school for over a year because his symptoms made it too difficult to attend.
I ran a complete panel for tick-borne infections, a comprehensive workup for mold exposure, and other general laboratory tests I order in chronic illness. Surprisingly, Aaron’s tests indicated he had bartonellosis, Lyme disease, past mold exposure, and hypothyroidism. I put him on an antimicrobial regimen, liothyronine for his low T3, and a detoxification protocol for mold.
Within a couple of months, Aaron was more engaged with his family and had the energy to begin home studies. After a few more months of treatment, he felt well enough to attend his senior year of high school. He was also able to wean off of two of his three psychotropic medications. His parents were thrilled to know Aaron’s anxiety, depression, and insomnia were not something he had to live with for the rest of his life.
Lyme Disease and Anxiety
Anxiety, like depression, is a common psychiatric symptom that can be associated with Lyme disease. Like other neuropsychiatric symptoms, anxiety is triggered by inflammation and the metabolic changes that occur in tick-borne infections. Concern about one’s health – especially if causes have not been identified – can also contribute to anxiety or panic disorders. Different types of anxiety can present in Lyme disease. These include hypervigilance, social anxiety disorder, panic disorder, obsessive-compulsive disorder (OCD), and post-traumatic stress disorder.
Of the tickborne co-infections, bartonellosis tends to cause an increase in anxiety. Bartonellosis requires a different treatment than Lyme disease, so it is important to test for all co-infections. I have seen generalized anxiety disorder and panic attacks resolve when patients are properly treated for Lyme disease and co-infections.
Of the associated tick-borne infections, Bartonella tends to contribute to anxiety more than the others.
Bartonellosis requires a different treatment than Lyme disease, so it is important to properly test for all co-infections. I have seen generalized anxiety disorder and panic attacks resolve when patients are properly treated for Lyme disease and co-infections.
Other Mood Disorders Associated with Lyme Disease
There are multiple neuropsychiatric conditions that have been associated with Lyme disease and other tick-borne infections. Some of these associations have been researched in controlled studies and published in medical journals, while others come from case reports or presentations at medical conferences by physicians who have treated thousands of patients with mood disorders.
Bipolar disorder has been associated with multiple infections, including Lyme disease.
People with bipolar disorder caused by Lyme disease tend to be rapid cyclers. In reports and studies, the incidence of bipolar occurred in 10%-28% of people with Lyme disease.
There have been at least 23 infections identified as one of the causes of autism.
Seven of these infections were tick-borne infections. Oftentimes other environmental and genetic factors play a role in the onset of autism spectrum disorder. Like other neuropsychiatric disorders mentioned previously, it is the immune response to the infection that results in inflammation that contributes to the symptoms. In one study of children diagnosed with autism and Lyme disease, 94% had previously tested negative for Lyme disease with the standard two-tiered CDC testing criteria.
Substance abuse and addiction can become part of someone’s life if they are suffering from chronic tick-borne infections.
This is especially true if the infections have been undiagnosed for a long period of time. I see this abuse or addiction most often in teenagers and young adults. This population may be suffering from fatigue, chronic pain, headaches, and anxiety or depression, and without a diagnosis, they turn to alcohol and/or recreational or prescription drugs to cope with the symptoms. Adults can also become addicted to pain medication. One report indicated substance abuse can range from 10%-33% of people with Lyme disease.
Schizophrenia and schizoaffective disorder are less common in people with Lyme disease.
However, in late-stage Lyme, paranoid symptoms occurred in 36% of patients. There was a slightly higher prevalence of hallucinations in people with Lyme disease in another report.
Psychiatrist Robert Bransfield has written about the association of Lyme disease and suicide.
Some individuals have been suffering from late-stage Lyme disease for an extended period of time. Whether or not they are being treated for the disease, some begin to lose hope they will ever get better. Most of the time, people are also suffering from anxiety, depression, bipolar disorder, or cognitive issues so their actions may be impulsive and unpredictable.
What Can Be Done About Neuropsychiatric Illness and Lyme Disease?
When someone is suffering from a mood or psychiatric disorder and the person is also experiencing additional symptoms such as fatigue, headaches, joint pain, insomnia, and cognitive issues, an underlying cause such as an infection should be ruled out. Other clues that there may be an infectious cause to psychiatric symptoms include having an “atypical” presentation of the diagnosis and not responding to common medications used to treat the mood disorder. Also, is there a possibility the person could have been exposed to ticks or other known vectors? Anyone who spends time outdoors, either where they live or vacation, or has pets that are indoor/outdoor is at risk for exposure to ticks.
If a tick-borne infection is the cause of a mood disorder, addressing the infection(s) can improve the mental symptoms. Those already on psychotropic medication may need to stay on the medication while the underlying cause(s) are treated. Immune and detoxification support to reduce inflammation is also effective at improving mental health.
Taking a comprehensive approach to identify and treat any underlying causes of psychiatric illness, especially in those with a multi-systemic and multi-symptomatic presentation. There is increased hope and improved outcomes for those suffering from what is otherwise a life-long disorder. Lyme disease and other tick-borne infections are more common than previously recognized and have a high likelihood of contributing to neuropsychiatric conditions.