Diagnosing acute Lyme disease is often straightforward. If someone develops flu-like symptoms following a tick bite or spending time in nature, the diagnosis of Lyme disease is often considered. However, when someone is sick with multiple symptoms for an extended period of time, it can take years to get a correct diagnosis. There are many nuances associated with Lyme disease testing. Read below to learn about accurate testing for chronic or late-stage Lyme disease.

How was Lyme Disease Testing Criteria Developed?
There may not be a more complex infection to diagnose than chronic Lyme disease. When Lyme disease was first discovered in the 1970s, the Center for Disease Control (CDC) wanted to track the number of cases in the US, so they developed diagnostic criteria for surveillance reporting to local public health departments. The criteria needed to be narrow to increase the sensitivity of cases reported. Unfortunately, the surveillance criterion made its way into doctor’s offices, and physicians began using the narrow criteria as diagnostic parameters for Lyme disease.
If someone had symptoms following a tick bite – or even years after a tick bite – but did not have a large bullseye rash, meningitis, facial paralysis, or encephalomyelitis, they were told they did not have Lyme disease.
Another limitation of the Lyme disease surveillance criteria is it only includes symptoms often seen in acute cases of Lyme disease and excludes many symptoms consistent with late-stage Lyme disease. Throw in the misconception that people can only contract Lyme disease in the northeastern U.S., and Lyme disease is not typically considered as a possible cause of symptoms in the rest of the country.
Poor Sensitivity of Traditional Lyme Disease Testing
If a physician is familiar with the many presentations of Lyme disease and considers Lyme disease as a possible diagnosis, standard laboratory testing has poor sensitivity so many cases are missed. The traditional laboratory test used to diagnose Lyme disease is a “two-tiered” test. This means an ELISA test is run first, and if it is positive, a second test called a western blot is performed to confirm the accuracy. If the ELISA test is negative, the western blot is not performed. The sensitivity of the ELISA test is so poor that it reports a false negative about half of the time. This means the more sensitive western blot never gets tested.
Physicians that specialize in treating tick-borne infections have historically considered the diagnosis of late-stage Lyme disease a clinical diagnosis. A clinical diagnosis is made if the patient has signs and symptoms consistent with a tick-borne infection and other diagnoses that could explain the signs and symptoms have been excluded. However, in recent years specialized laboratory testing has advanced and should be used to confirm a suspected diagnosis.
In many scenarios other possible diagnoses have been ruled out, there has been a possible exposure to ticks (including the distant past with chronic Lyme disease), and the pattern of symptoms is consistent with Lyme disease. Specialized laboratory testing is more sensitive than general reference laboratory testing (LabCorp, Quest, etc.) and should be used to confirm the diagnosis.
Additional Challenges with Lyme Disease Testing
Another obstacle with many Lyme disease tests are they rely on detecting antibodies produced by the immune system against the bacteria that causes Lyme disease. In some circumstances, the level of antibodies may be low due to immune suppression which compromises the accuracy of the test. In addition, if a test is performed too soon after a tick bite, antibodies may have not yet formed. If antibiotics are taken early in an infection, the medication can prevent antibody formation resulting in future negative tests.
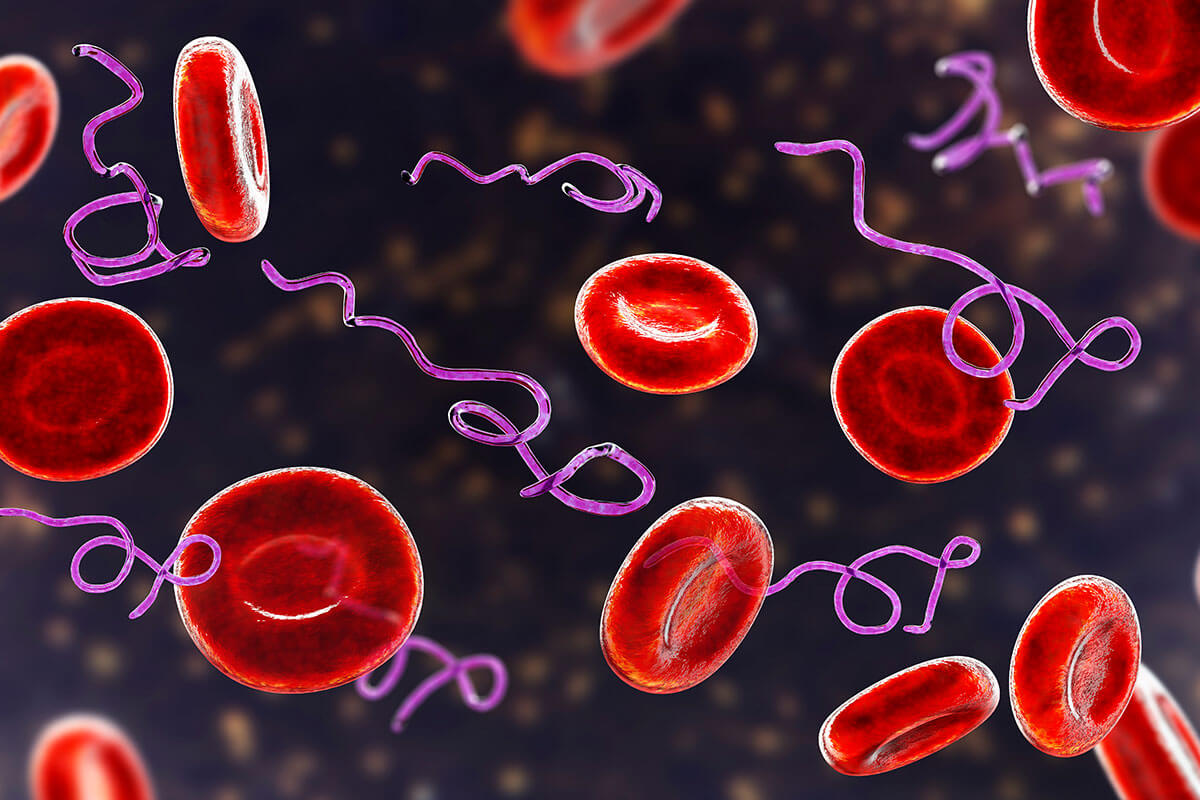
In late-stage Lyme disease, the Lyme spirochete has burrowed into tissues like muscles, joints, and organs. The bacteria can also form a protective structure around itself called a biofilm. These “immune-privileged” locations prevent the immune system from detecting the bacteria so antibodies are not formed for the test to detect.
ELISA (Enzyme-Linked Immunosorbent Assay)
ELISA methodology of testing works by attaching Lyme antigens to a surface in a laboratory. If a blood sample has Lyme antibodies, the antibodies will bind to the antigen. This creates an antigen/antibody complex that is linked to an enzyme (which is another antibody). In the last step, a substrate is added that allows the result to be measured.
The limitation of the ELISA test is the cut-off for a positive result is set extremely high to make the test highly specific. However, the high specificity comes at the cost of the sensitivity of the test. A review of research studies looking at the sensitivity of ELISA testing for Lyme disease revealed it is accurate less than half the time. Because of this, the standard two-tiered test for Lyme disease should not be relied upon to diagnose Lyme disease.
Immunofluorescence Assay (IFA)
Like the ELISA, the IFA methodology for Lyme disease testing is an indirect test that looks for antibodies formed against the bacteria that causes Lyme disease – Borrelia burgdorferi. In the laboratory, blood is added to a slide that contains the Borrelia antigens. If the blood contains antibodies to Borrelia, the antibodies will bind to the antigens on the slide. The final step is to view the slide under a fluorescent microscope (hence the name). Antibodies bound to the antigens will light up if they are present.
The IFA lacks specificity and sensitivity, so it is not a preferred method for diagnosing Lyme disease. Antibodies from other infections can bind to the antigens on the test strip (called cross-reactivity) leading to a false-positive result.
The Western Blot for Lyme Disease
The western blot is also an antibody-based test but is more sensitive and specific than the ELISA and IFA tests. Specific proteins that are on the outer surface of Lyme bacteria are produced on strips for this test. If there are Lyme antibodies in a blood sample they will bind to the surface protein antigens. The pattern of binding indicates whether or not the result is positive. In Lyme disease, there are specific outer surface proteins (called bands), and the specific pattern formed on the blot increases the specificity of the test.
The outer surface proteins are numbered by weight in kilodaltons. Specific bands for Lyme disease include 23-25 kDa, 31 kDa, 34 kDa, 39 kDa, 41 kDa, and 83-93 kDa. The CDC criteria require at least two of three positive IgM bands and five out of ten positive IgG bands for a western blot result to be positive. The CDC criterion is stringent so some Lyme specialty laboratories have established more inclusive criteria based on thousands of tests performed.
If someone had a possible exposure to ticks, had clinical signs and symptoms of Lyme disease, but did not have the exact pattern considered to be positive by the CDC, they were told by their doctor they do not have Lyme disease.
A limitation of the CDC criteria is bands 31 and 34 are not included in the diagnosis. The CDC excludes these two bands because a person might be positive if they received a Lyme vaccine. Ironically, very few people received the Lyme vaccine when it was available for only a couple of years before it was removed from the market due to adverse reactions (and lawsuits). Based on over 25 years of experience and validation studies, the Lyme specialty laboratory Igenex requires two out of six bands to be positive for an IgM positive result.
Western blot tests offered by commercial laboratories such as Quest and LabCorp develop their testing strip using a synthetic laboratory strain of Borrelia called B31. Igenex uses the synthetic B31 strain as well as the wild (occurs in nature) 297 strains to increase the sensitivity of their western blot.
Because Igenex uses more inclusive criteria than the CDC and two strains of Borrelia for testing, their western blot may diagnose Lyme disease that is missed by less sensitive commercial laboratories.
ImmunoBlot for Lyme Disease
The Lyme immunoblot uses recombinant proteins on the blot so it is more sensitive than the western blot. This test can detect Lyme disease as early as one week after exposure to the Borrelia bacteria and detect late-stage Lyme when antibodies are typically low. Like the western blot, an immunoblot result has to meet certain criteria for a positive result.
Additional species of Borrelia bacteria fall into the Tick-Borne Relapsing Fever Group (TBRF). The TBRF group causes symptoms similar to Lyme disease, and some species may be more common in other parts of the United States, like California. This may be why some Californians test negative on a traditional Lyme test.
Immunoblot testing is also available for multiple Babesia and Bartonella species. The panel of tests I most commonly use in my practice includes Lyme, TBRF, Babesia, and Bartonella immunoblots
T-Cell Testing
In recent years, the sensitivity of T-cell testing for Lyme disease has improved. This methodology detects an immune cell (called a T-lymphocyte) that has formed in response to the Borrelia bacteria. T-cells are part of the innate immune response, unlike antibodies that are created as part of the adaptive immune response.
Early in infection, T-cells develop before antibodies are formed, so a T-cell test may help detect early Lyme disease. As the disease progresses, some people’s immune system does not convert from an innate to an adaptive response. This inhibits antibody formation, so a T-cell test would be helpful in this scenario.
Lyme Disease Culture
All of the above tests are considered indirect because the laboratory test is looking for an immune response to the bacteria. There are limitations to indirect testing making it difficult to get an accurate diagnosis. For example, an elevated IgG antibody may reflect a past infection and does not confer an active infection. One of the great debates in chronic Lyme disease is whether or not the infection is active or if symptoms are caused by something else, like immune-mediated inflammation.
Direct testing methodology is the gold standard for determining if an infection is active. There are a few direct tests for Lyme bacteria, but the sensitivity of these tests has historically been poor because the bacteria rarely circulates in the bloodstream. In February 2023, Igenex Laboratory introduced a new direct test called culture-enhanced PCR. Blood is stored in a unique culture medium for two weeks and then analyzed by PCR. Validation studies for the specificity of the cePCR test were high. Direct testing may be more accurate when bacteria levels are highest, including early in infection or during a symptom flare. The cePCR is also available for TBRF, Bartonella, and Babesia.
Putting Lyme Disease Testing Together
Late-stage Lyme disease can be difficult to diagnose. The CDC criterion was established for surveillance purposes only, so should not be used for diagnostic purposes. Lyme disease tests from commercial and hospital laboratories have poor sensitivity and specificity.
Laboratories that specialize in Lyme disease testing provide more accurate results and should be used when attempting to determine if Lyme disease is the cause of symptoms. Specialty laboratories should also test all co-infections since they can cause similar symptoms and may interfere with Lyme treatment. No one testing method is perfect, so laboratory results need to be taken into consideration by a Lyme-literate physician. Any treatment plan is only as effective as the accuracy of the lab results.