Exposure to water-damaged buildings (WDB) and mold has been linked to various health issues, including chronic fatigue syndrome (ME/CFS), immune system dysregulation, and neurological dysfunction. A growing body of research suggests that sinus colonization in mold illness, facilitated by biofilm formation, plays a crucial role in the persistence of these illnesses, even long after the initial exposure. This article illustrates the connection between mold exposure, sinus colonization, and chronic symptoms, emphasizing the importance of effective sinus treatment for recovery.
The Sinus: A Breeding Ground for Mold
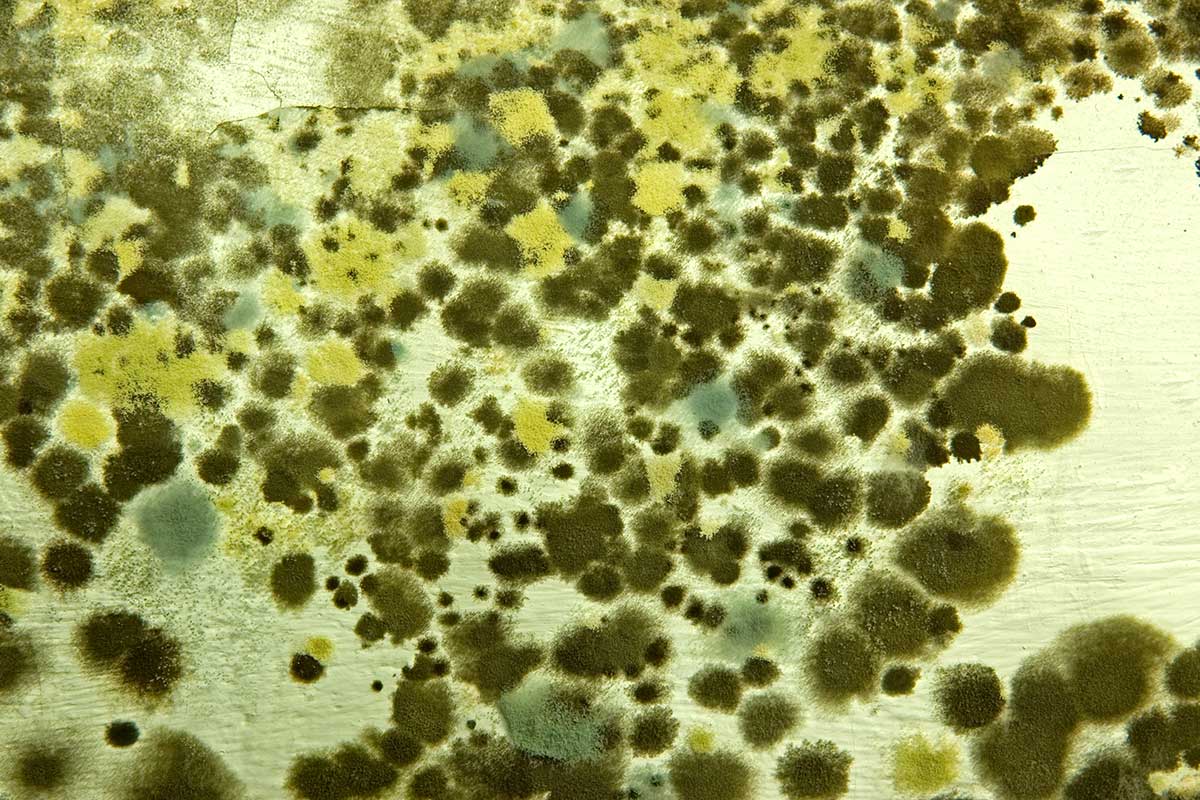
The nose and paranasal sinuses, while typically home to numerous fungal species, become vulnerable to colonization by mycotoxin-producing molds upon exposure to mold-contaminated environments. Common culprits include Aspergillus, Penicillium, Chaetomium, Fusarium, and Stachybotrys species, many of which have the potential to produce mycotoxins and contribute to chronic illness. These opportunistic molds can establish themselves within the sinus cavities, taking advantage of the warm, moist environment.
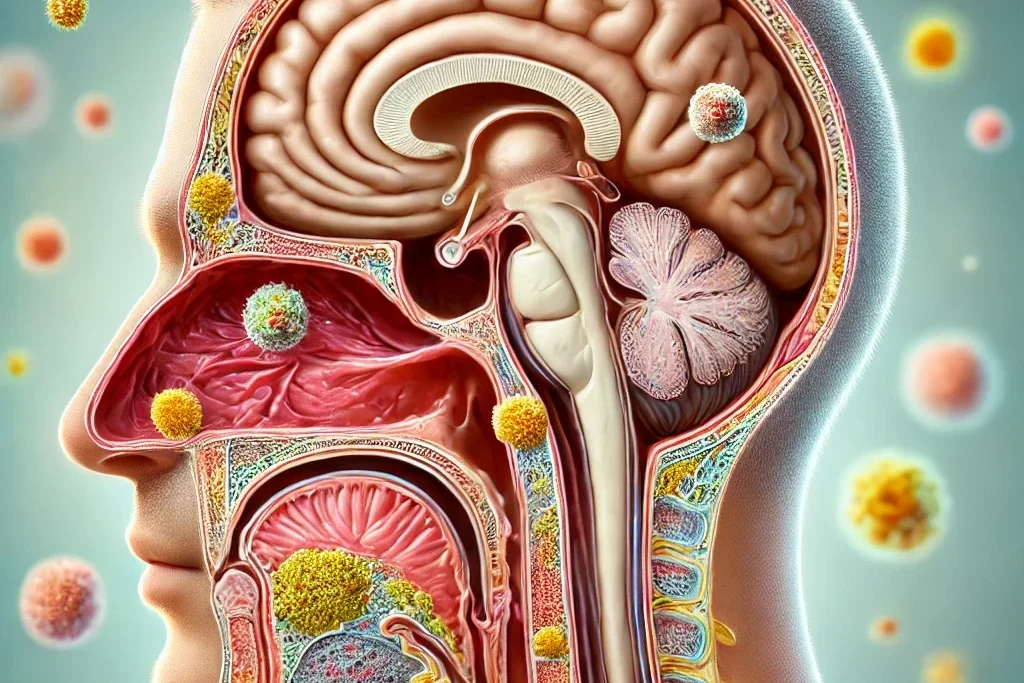
The Sinus-Brain Connection
Paramount to the sinuses being the perfect breeding ground for mold to colonize, their proximity to the brain contributes to neuroinflammation. Inflammatory cytokines in the sinuses produced by molds and mycotoxins migrate along the olfactory nerve into the brain. Inflammation in the brain can lead to mold-related neuropsychiatric symptoms, including headaches, brain fog, anxiety, depression, and insomnia.
Biofilms: Shielding Mold and Perpetuating Illness
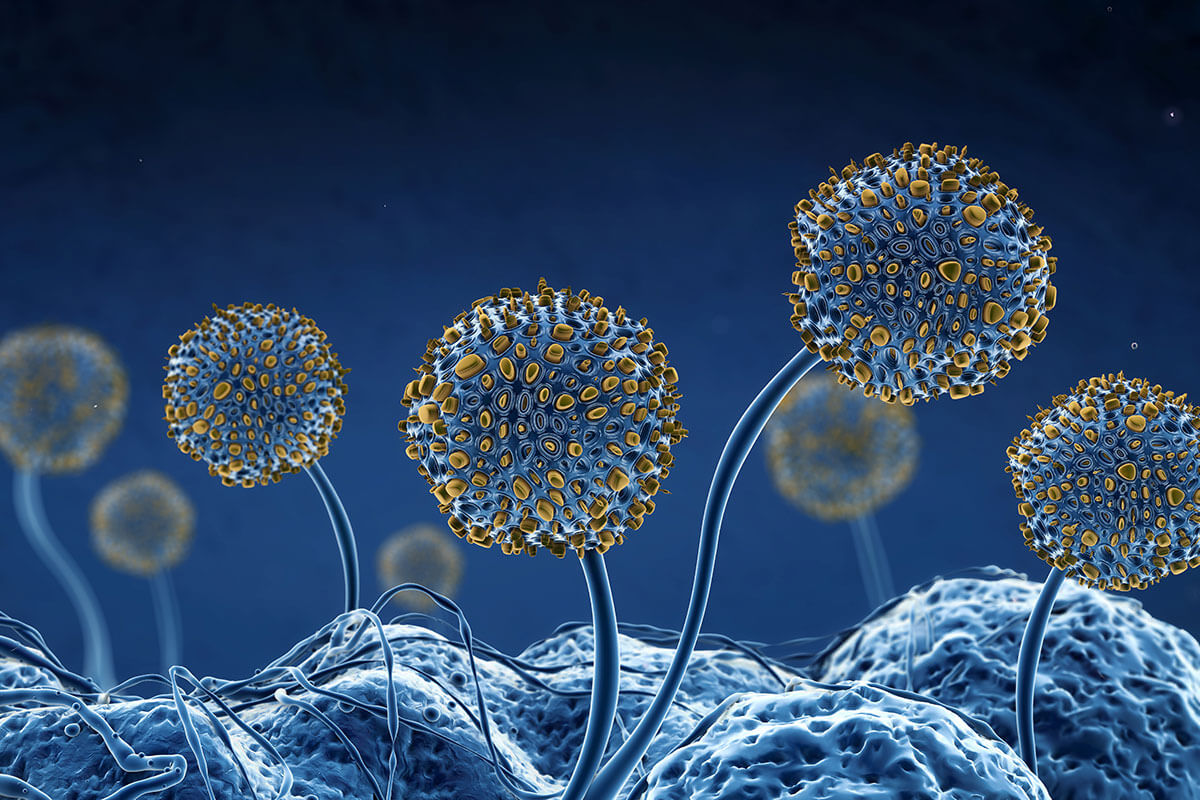
A key factor in the persistence of mold in the sinuses and the resulting chronic symptoms is the formation of biofilms. Biofilms are complex, structured communities of microorganisms, including mold, encased within a protective matrix. The matrix is composed of various substances, including polysaccharides, fibrin, and even mycotoxins. Biofilms provide several advantages to mold, allowing it to thrive and evade the body’s defenses:
Protection from the immune system and antifungal treatments
The biofilm acts as a physical and chemical barrier, making it difficult for the immune system’s cells and antifungal medications to penetrate and effectively eliminate the mold. This protective shield enables mold to persist despite treatment efforts, contributing to chronic inflammation and ongoing release of mycotoxins.
Enhanced mycotoxin production
Research indicates that mold embedded in biofilms can produce more mycotoxins than free-living mold. This heightened mycotoxin production exacerbates the patient’s illness and complicates treatment efforts.
Persistence and chronic inflammation
Biofilms’ resilient nature allows mold to persist in the sinuses, leading to chronic inflammation and a constant source of mycotoxins. This ongoing inflammation and mycotoxin exposure contribute to the development and persistence of chronic symptoms.
The Link Between Sinus Colonization and Chronic Symptoms
The presence of mycotoxin-producing mold in the sinuses is not merely a localized issue; it has far-reaching consequences for overall health. When released by mold, mycotoxins can readily cross the nasal and sinus mucosa and enter the bloodstream, affecting various organs and systems throughout the body. This systemic spread of mycotoxins can explain the diverse symptoms experienced by individuals with chronic mold illness.
Studies have shown that mycotoxins can be detected in the urine of chronically ill patients, even years after their initial exposure to water-damaged buildings.
This finding strongly suggests the existence of an internal reservoir of mold, continuously producing and releasing mycotoxins into the body. The sinuses, with their propensity for mold colonization and biofilm formation, represent the most likely site for this internal reservoir.
Chronic Sinus Infections: Bacterial or Fungal?
Over the years, I have seen patients with a history of recurrent chronic sinus infections. Some have had sinus surgeries to correct their chronic symptoms; only the surgeries were unsuccessful. In 1999, a group of physicians from the Mayo Clinic conducted a study to determine the incidence of fungal sinusitis in people with chronic sinusitis. They discovered that 96% of nasal secretions in people with consecutive chronic sinusitis had positive fungal cultures. Fungal cultures are not commonly ordered by ENT physicians, so people with chronic sinusitis are typically prescribed antibiotics.
Addressing Sinus Colonization: A Key to Recovery
Recognizing the significant role of sinus colonization in chronic mold illness, effective sinus treatment becomes a cornerstone of recovery. While traditional treatments for chronic sinusitis often focus on addressing bacterial infection and inflammation, they may fall short in effectively targeting the underlying mold colonization and biofilm formation.
Intranasal antifungal therapy has emerged as a promising approach for directly combating mold colonization in the sinuses.
Itraconazole and Amphotericin B have demonstrated efficacy against a broad spectrum of mold species, including those commonly found in the sinuses. Moreover, studies have shown that amphotericin B can penetrate and disrupt biofilms, reaching the embedded mold. While itraconazole may be less effective against biofilms, it can still provide clinical benefit when combined with biofilm-disrupting agents.
In my practice, I frequently prescribe a compounded formula consisting of itraconazole or amphotericin B and EDTA. Occasioanlly, I will also combine budesonide and mupirocin. The formula is mixed with sterile saline and administered through a nebulizer (NasoNeb works best), allowing targeted delivery of the medication to the sinuses. This localized delivery minimizes systemic absorption and potential side effects while maximizing the antifungal effect within the sinus cavities.
Key observations from studies on intranasal antifungal therapy include:
- Significant clinical improvement: Many patients treated with intranasal antifungal medication have reported clinical improvement, with reductions in various symptoms, including fatigue, headache, cognitive dysfunction, and sinus-specific symptoms. Some patients have experienced marked reductions in symptoms, achieving a near-complete resolution of their chronic illness.
- Decreased mycotoxin levels: Urine mycotoxin levels have been shown to decrease substantially in patients who responded well to intranasal antifungal therapy, supporting the link between sinus colonization, mycotoxin production, and clinical symptoms. This decrease in mycotoxin levels provides objective evidence of the treatment’s effectiveness in reducing the body’s mycotoxin burden.
- Importance of biofilm disruption: Combining antifungal therapy with agents that disrupt biofilms is crucial for maximizing treatment efficacy. Agents like EDTA can help break down the biofilm’s protective matrix, allowing the antifungal medication to reach the embedded mold more effectively.
Voriconazole, another broad-spectrum antifungal, has shown efficacy in treating invasive fungal infections and may also be beneficial for addressing mold in the sinuses.
The Need for Long-Term Management
While intranasal antifungal therapy offers considerable promise for recovery from chronic mold illness, relapse is possible, especially if treatment is discontinued prematurely. The protective nature of biofilms and the potential for residual mold to re-establish itself necessitate a long-term management approach.
Some patients may achieve long-term remission with a course of treatment, while others may require maintenance therapy to prevent relapse. Factors influencing the duration of treatment include the extent of sinus colonization, the severity of biofilm formation, and the individual’s immune response.
Close monitoring of symptoms and mycotoxin levels is essential for guiding treatment decisions. Regular follow-up appointments with a healthcare professional knowledgeable in mold illness are crucial for assessing treatment progress, identifying potential relapses, and adjusting therapy.
A Comprehensive Approach to Recovering From Mold Illness
Mold exposure and subsequent sinus colonization are significant contributors to the persistence of mold-related illness. Understanding the protective role of biofilms in harboring mold and enhancing mycotoxin production is crucial for effective treatment. Nebulized treatment with antifungal medication and biofilm-disrupting agents offers a promising approach for addressing mold colonized in the sinuses. This targeted therapy can reduce mold levels, decrease mycotoxin burden, and improve symptoms.