Mast cells are a part of the human immune system and protect against foreign invaders. Mast cells are concentrated in areas where the external environment comes into contact with the human body, such as the skin, the lungs, the mucous membranes inside the nose, and the gastrointestinal tract. In normal circumstances, mast cells release various compounds called mediators in response to foreign substances to keep us safe. In mast cell activation syndrome (MCAS), there is an inappropriate release of the chemical mediators that can cause inflammatory symptoms anywhere in the body. Many people (including physicians) mistakenly refer to these symptoms as histamine intolerance when MCAS is the cause.
What Causes Mast Cell Activation Syndrome?
For some people, mast cells are more prone to release their mediator contents. However, for many, there is an underlying cause (or causes) that increases the risk of developing mast cell activation syndrome.
Causes of MCAS include:
- Bacterial infections
- Viral infections
- Fungal infections
- Heavy metals
- Herbicides
- Mold illness
- Allergens – food and environmental
- Genetically predisposed
Additionally, certain triggers cause mast cells to degranulate and release mediators in individuals who are susceptible.
MCAS triggers are:
- Heat
- Stress
- Exercise
- Physical trauma
- Alcohol
- Foods
- Hormonal changes
- Medications
- Odors
- Insect stings
This article aims to provide you with information you can use (or take to your physician to help you) to improve the outcome of your symptoms or illness. In this article, I share my clinical experience in treating MCAS. I also highlight important information from published research studies on MCAS to help you better understand the nature of MCAS and how to get properly tested.
Mast Cells Release Chemical Mediators
Inside each mast cell, there are tiny sacs called granules. Granules contain up to a couple of hundred chemical mediators that get released when a trigger, such as an allergen or toxin, binds to a mast cell. Histamine is the most common mediator released from mast cells in response to an allergen such as pollen. Other mediators include tryptase, heparin, prostaglandins, leukotrienes, and cytokines. Different mediators can cause a unique physiological reaction in the surrounding tissue. For example, tryptase is a proteolytic enzyme and can break down nerve endings.
Who is at Risk for Mast Cell Activation Syndrome?
Since mast cells are present in all humans, there is the potential anyone can develop mast cell activation syndrome. People who have developed immune dysfunction from chronic infections, toxin exposure, repeated allergen exposure, and individuals with genetic variations are at an increased risk of developing MCAS.
One study reported on over 400 patients with MCAS and identified the prevalence of specific characteristics. Women made up 69% of patients with mast cell activation syndrome, and 75% were Caucasian. The most frequent age at onset of symptoms was nine years old, and in most patients, it took 30 years to get a diagnosis of MCAS. This implies people with MCAS may spend a good portion of their lives without a proper diagnosis. Other surveys have confirmed that females have an increased incidence of MCAS.
Symptoms of Mast Cell Activation Syndrome
After receiving a diagnosis of mast cell activation syndrome in adulthood, many people realize the symptoms they have experienced since childhood were related to MCAS. It is common for children (and their parents) to be told by their pediatrician that they will “outgrow” their symptoms. Because mast cells are located throughout the body and contain over a hundred inflammatory compounds, symptoms can occur in every organ system. This multi-symptom, multi-system involvement, and because mast cell activation syndrome is not well-recognized, creates an extreme challenge for physicians to diagnose.
The most common MCAS symptoms are:
- Systemic – fatigue, sensitivity to food and medication
- Respiratory – nasal congestion, shortness of breath, asthma, throat swelling
- Neurological – headaches, migraines
- Mental/emotional – decreased concentration, memory; anxiety, depression
- Musculoskeletal – aches, bone pain, osteoporosis
- Digestive – nausea, vomiting, heartburn (GERD), diarrhea, abdominal cramps
- Skin – flushing, itching, hives, temperature dysregulation
- Cardiovascular –high and low blood pressure, lightheadedness, racing heart, hypercoagulation
- Genitourinary – irritable bladder, interstitial cystitis
Conditions Associated with Mast Cell Activation Syndrome
There are several conditions associated with mast cell activation syndrome. It can be difficult to distinguish if the illness or disease has caused MCAS or if MCAS has caused symptoms that present like the illness or disease.
Conditions associated with MCAS include:
- Chronic Lyme disease
- Fibromyalgia
- Autism
- Hypercoagulation
- ME/CFS (chronic fatigue syndrome)
- Irritable bowel syndrome (IBS), small intestine bacterial overgrowth (SIBO), Leaky gut syndrome
- Mold illness
- POTS/Dysautonomia
- Ehlers-Danlos hypermobility
- Multiple chemical sensitivity
- Autoimmune conditions
Mast Cell Activation Syndrome in Digestive Disorders
Mast cells are highly concentrated in the gastrointestinal tract to protect humans from any foreign invaders they may swallow. Whether triggered by bacteria, parasites, or food allergies, mast cell activation in the gut can contribute to digestive symptoms such as heartburn, nausea, vomiting, constipation, and diarrhea. Digestive conditions associated with MCAS include IBS, small intestine bacterial overgrowth (SIBO), eosinophilic esophagitis, and leaky gut syndrome.
Researchers tested patients with persistent IBS-like symptoms for mast cell activation syndrome (MCAS) and small intestine bacterial overgrowth (SIBO). The results revealed that for all patients who tested positive for MCAS, 66% experienced digestive symptoms before any other MCAS symptoms.
The most common symptoms these patients experienced were abdominal pain (87%), bloating (75%), constipation (67%), nausea (62%), and heartburn (54%).
SIBO was present in 31% of patients with MCAS, and the authors concluded that mast cell mediators in the gut may contribute to altered digestive motility, which could lead to SIBO.
A significant number of my patients with MCAS have reported that they react with digestive or systemic symptoms to many foods, so they have to eat a limited diet. This reaction is caused by antibodies that have been formed against certain foods and then bind to mast cells.
There may also be increased inflammation in the small intestine from increased mast cell activity. Small intestine inflammation (also termed leaky gut syndrome) allows food particles to easily cross the intestinal barrier, enter the bloodstream, and trigger an immune response. In my experience, when mast cell activation and leaky gut syndrome are effectively treated, people can eat a more varied diet without experiencing adverse reactions.
High Histamine Foods
Certain foods are high in histamine or cause histamine release from mast cells. Below is a list to guide you to help you identify which foods cause a reaction in your body. In general, there is a direct correlation between the reduction of high-histamine and histamine-releasing foods and the improvement in MCAS symptoms.
High histamine foods
- Fermented foods – kombucha, miso, kimchi, sauerkraut, soy sauce
- Pickles and pickled vegetables
- Dairy – aged cheese, yogurt, sour cream, kefir
- Vinegar – possibly in salad dressings, mayonnaise
- Cured meats – deli meats, salami, ham, sausages
- Vegetables – tomatoes, eggplant, spinach
- Nuts – peanuts, cashews
- Alcohol – wine, beer, champagne
- Fish – herring, smoked mackerel, sardines, tuna, anchovy
- Bone broth
- Citrus fruit
- Chocolate
Foods that cause histamine release
- Citrus fruit
- Fish
- Papaya, strawberry, pineapple
- Alcohol
- Peanuts
- Tomatoes, spinach
- Chocolate
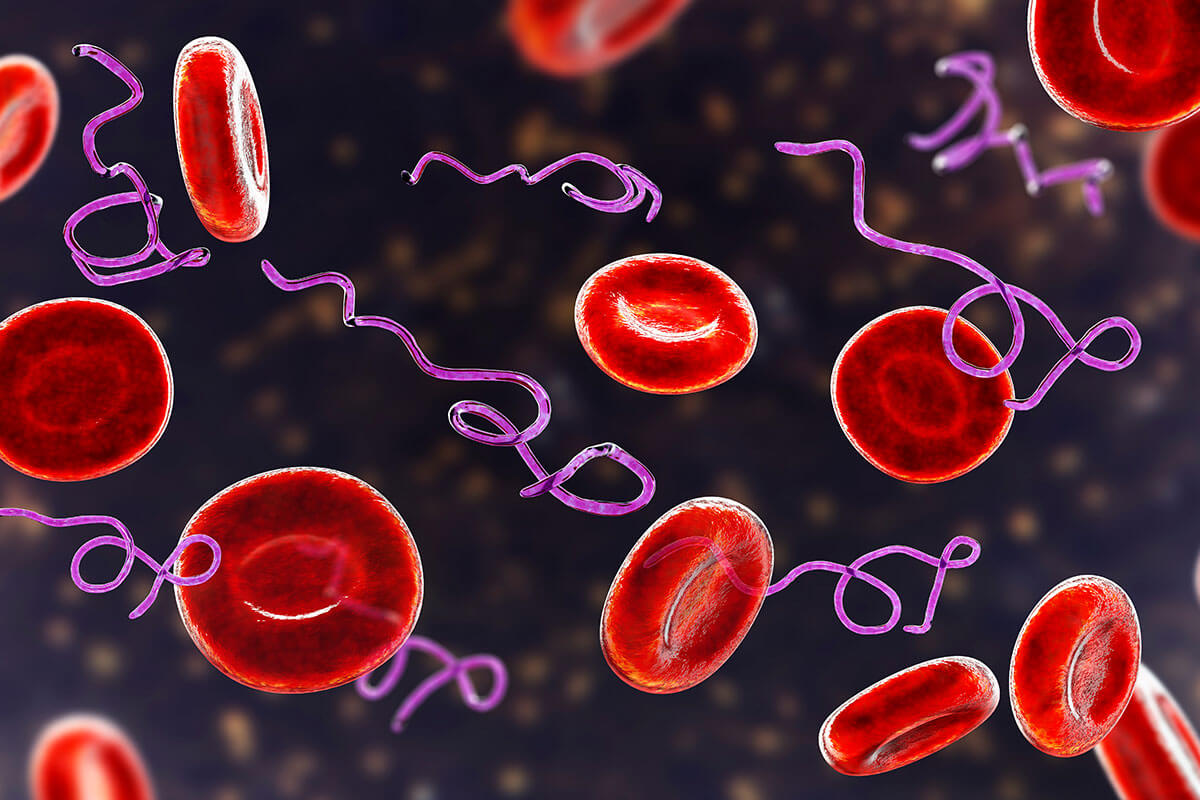
Lyme Disease is Associated with Mast Cell Activation Syndrome
Pathogens, including viruses, bacteria, fungi, and parasites, can contribute to mast cell activation syndrome. The mast cell reaction is an immune response that attempts to protect humans from pathogens.
About half of the patients I see with tickborne infections also experience MCAS. Many symptoms of MCAS overlap with Lyme disease, and effectively treating MCAS not only helps the patient feel better, but it also helps to clarify what symptoms remain from Lyme disease.
When Lyme bacteria, or other pathogens, and mast cell activation syndrome are present, MCAS is part of the immune dysregulation and contributes to symptoms. A research study confirmed that the Lyme bacteria trigger the degranulation of mast cells. I prefer to approach treating illnesses and diseases by addressing their root causes. It is essential to test for Lyme disease and associated infections to determine if these infections are contributing to the release of mast cell mediators.
Mold Exposure Can Cause Mast Cell Activation
Human exposure to environmental molds and their toxins (mycotoxins) cause immune dysfunction and immune suppression. Mold and mycotoxins are also involved in mast cell activation syndrome. Suppose someone is experiencing any MCAS symptoms and has been exposed to a water-damaged building or environmental mold. In that case, it is crucial to properly test for mold illness. Addressing mold toxicity helps to improve the outcome of mast cell activation syndrome.
Diagnosing Mast Cell Activation Syndrome
The clinical symptoms of mast cell activation syndrome should clue the physician in to order laboratory tests to confirm this suspicion. Multiple diagnostic criteria for mast cell activation syndrome have been proposed by mast cell researchers, physicians, and organizations. The Consensus 2 Criteria is the most accurate approach for testing MCAS.
The most significant challenge in diagnosing MCAS with laboratory testing is the proper handling of blood and urine samples. The samples require constant chilling to maintain stability. A 24-hour urine sample is collected at home before the blood draw. It is kept in the refrigerator and transported in a cooler to the lab. The laboratory phlebotomist also needs to be aware of keeping the samples chilled at the time of the blood draw. Proton pump inhibitors (Prevacid, Prilosec, etc.) and NSAIDs (Advil, Tylenol, etc.) need to be avoided five days before testing.
Even if the specimens are handled properly, it can be challenging to see even one mediator elevated due to the timing of mast cell degranulation. One approach is to collect the samples during a flare of MCAS symptoms.
The diagnostic workup for MCAS includes:
- Tryptase, serum (frozen)
- Chromogranin A, serum (chilled)
- Prostaglandin D, plasma (chilled)
- Heparin, plasma (chilled)
- Histamine, plasma (chilled)
- Leukotriene E4, urine (chilled)
- N-methylhistamine, urine (chilled)
- 11B Prostaglandin F2, urine (chilled)
Click here to download and print a list of MCAS tests and handling instructions for your physician or lab.
Is it Mast Cell Activation Syndrome?
Mast cells are located throughout our bodies and are an essential part of our immune system. There has been an increased awareness and incidence of mast cell activation syndrome in the past decade. If you have symptoms consistent with MCAS, it is essential to undergo proper testing for the above mediators. For many people, the underlying causes of mast cell activation syndrome may include mold-related illness, chronic viral or bacterial infections, and exposure to environmental toxins. It is critical to identify potential causes through proper testing to improve symptoms and the outcome of treating mast cell activation syndrome.