Bartonellosis, the infection caused by the bacteria Bartonella, is possibly a more problematic human infection than Lyme disease. Like Lyme disease, Bartonella can be transmitted to humans through a tick bite. However, Bartonella can also be transmitted to humans by various other vectors. Historically, testing for Bartonellosis has been insensitive. Bartonella causes symptoms similar to Lyme disease but requires different treatment, so it is important to test for it properly. However, the biggest concern Bartonella poses over Lyme disease is most physicians are entirely unaware of this prevalent bacteria.

What is Bartonella
Bartonella commonly occurs with Lyme disease, so it is referred to as a tickborne co-infection. About 30 species of Bartonella bacteria have been identified, but not all species cause disease in humans. Bartonella is a gram-negative bacteria – meaning it has two cell walls – that infects human cells, allowing it to hide from the immune system and disrupt normal cellular function.
Bartonella is the Cause of Cat Scratch Disease
Cat scratch disease is the most well-known disease caused by Bartonella henselae. Cat fleas carrying Bartonella bacteria defecate on cats, and the bacteria will survive in the feces on cats for many days. When cats scratch themselves, the bacteria from the feces get under their claws, then transmitted to humans through a scratch. Bartonella bacteria have been identified in cat saliva and can be transmitted by a cat bite.
How is Bartonella Transmitted?
It is accepted that ticks transmit the bacteria that cause Lyme disease. However, it was not until 2008 when an article was published in a medical journal that brought awareness to tick transmission of Bartonella.
Other vectors that infect humans with Bartonella are sandflies, lice, and fleas. An estimated 6-12 million children between the ages of 3 and 11 get head lice each year, but this number is grossly underestimated since lice is not a reportable infection. Mosquitoes have been implicated as a vector of Bartonella. A case report in the medical literature indicates spider bites transmitted Bartonella to multiple members of a family that went on to develop neurological symptoms.
With this many vectors that transmit Bartonella, it is easy to see why Bartonellosis should be a global health concern.
Bartonella in California
Contrary to conventional medical belief, Bartonella bacteria exist in ticks in California. In 2001, researchers from U.C. Davis collected western black-legged ticks (Ixodes pacificus) from three locations in Santa Clara County. Of the ticks collected, a remarkable 19.2% tested positive for Bartonella.
A year later, some of the same researchers conducted another study of ticks from six counties in northern and southern California. This time they looked at the western black-legged tick and the Pacific Coast tick (Dermacentor occidentalis). Bartonella DNA was found in 11.6% of the ticks. None of the ticks from Los Angeles County were positive for Bartonella, contributing to a lower percentage than the previous study. This was the first study that detected Bartonella in nymphal western black-legged ticks.
In 2006 researchers tested western black-legged ticks for Bartonella, Borrelia (Lyme disease), and Anaplasma from Santa Cruz County. This study identified 6.5% of ticks tested were positive for Bartonella.
Squirrels in California are a frequent reservoir host of Bartonella. In 2016 researchers tested squirrels and their fleas from seven counties in California for a particular species of Bartonella. Surprisingly, 69% of the squirrels and 31% of the fleas tested positive for Bartonella. The same year, another research group tested squirrels from two northern California counties for Bartonella. Like the other group’s findings, 71% of squirrels harbored Bartonella bacteria. Since squirrels live in urban, suburban, and rural areas, these findings raise the level of concern about Bartonella transmission to humans.
How Does Bartonella Cause Symptoms?
Bartonella bacteria are transmitted to humans through a bite from a vector or a cat scratch. In lice, the transmission of Bartonella to humans occurs when lice feces enters a break in the skin when a person scratches their scalp.
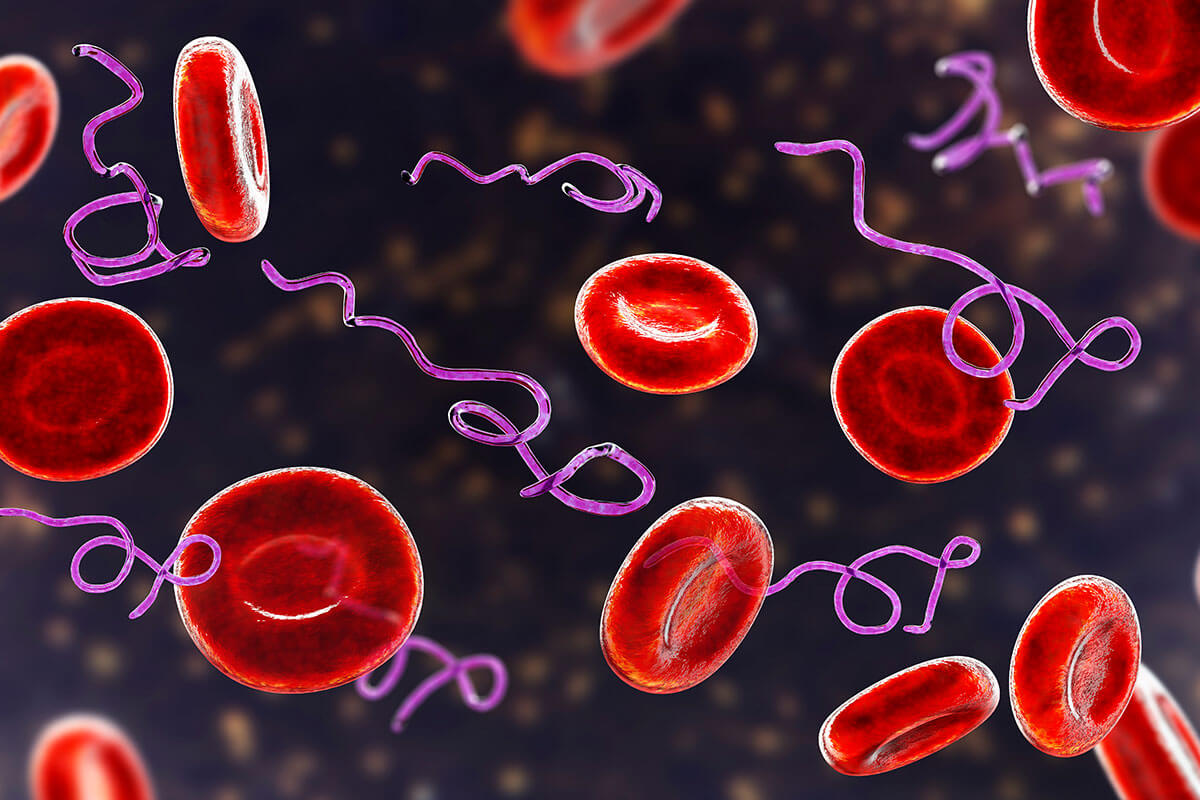
“One of the most fascinating aspects of a Bartonella infection is the intracellular parasitism of erythrocytes (red blood cells), a practice termed hemotrophy.” Pestilence, persistence, and pathogenicity: infection strategies of Bartonella.
Once in the bloodstream, the bacteria attach to red blood cells. Bartonella possesses specific proteins, enzymes, and genes that allow the bacteria to invade red blood cells. Inside the cell, the bacteria replicate and then are released from cells, where they are transported to organs and tissues that are highly vascularized, such as the heart, liver, spleen, and blood vessels. In Bartonella Quintana, bacteria may be released from red blood cells every five days, causing a cyclical pattern of symptoms.
The severity of infection with Bartonella is determined by the virulence of the bacteria species, the bacterial load, and the health of the infected person’s immune system. It is the host’s immune response that determines the outcome of the infection.
Bartonella Contributes to Small Vessel Disease
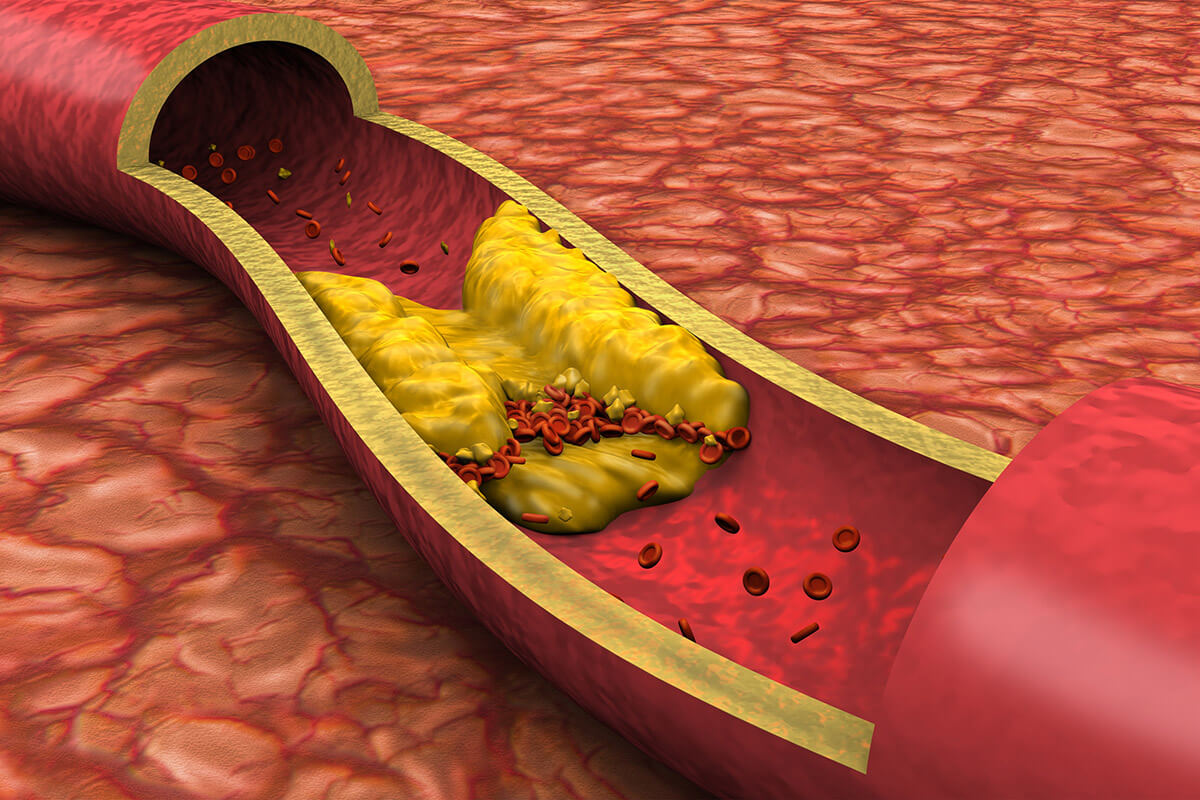
Bartonella prefers the cells that line blood vessels called endothelial cells. Bacteria inside of the vessel wall create inflammation and fibrin deposition, causing narrowing of the vessel where blood flows. Blood vessel constriction reduces blood flow and oxygen delivery to organs and tissues. Decreased oxygen causes tissue damage and leads to loss of function in cells contributing to symptoms. Tissue that receives blood from small vessels like capillaries is most at risk.
The central nervous system – especially the brain – is susceptible to decreased oxygen delivery. The brain’s white matter does not have collateral circulation, so neurological symptoms manifest early in infection with Bartonella. Symptoms such as cognitive impairment, disconnection syndrome, poor executive function (decisions, planning), decreased working memory, delayed processing speed, and mood swings are associated with small vessel disease caused by Bartonella.
Symptoms of Bartonella
- Neurological – headaches, peripheral neuropathy (numbness, tingling in hands, feet), dysautonomia/POTS, tremors, seizures, vertigo, PANS/PANDAS, OCD, ALS
- Psychological – cognitive impairment, decreased processing speed, hallucinations, disconnection/dissociation, Schizophrenia, depression, anxiety, panic attacks, agitation, mood swings
- Musculoskeletal – pain in the soles of the feet, arthritis, rheumatoid arthritis, bone pain, joint hypermobility, muscle weakness, muscle twitching
- Immune – swollen lymph nodes, frequent sore throats, fevers (especially of unknown origin)
- Blood – anemia, low platelets (thrombocytopenia)
- Visual – blurred vision, retinitis
- Skin – stretch marks (especially horizontal on back and hips)
- Abdominal – enlarged liver and spleen (hepatosplenomegaly, pain under the ribcage), liver cysts
- Cardiovascular – endocarditis, palpitations
- General – fatigue, insomnia, nausea
Bartonella is a Stealth Infection
Bartonella invades and resides inside of red blood cells. This strategy prevents Bartonella from being detected by the infected person’s immune system. Like many other low-grade, chronic infections, Bartonella shares DNA with other bacteria to improve its survival. As bacteria genetically shift, they can persist inside human hosts by evading the immune system.
“Bartonella characteristically avoids elicitation of a host immune response by means of passive camouflage and active deception as part of its stealth infection strategy. This bipartite strategy of “anti-immunology” aims at colonization of the erythrocytic niche, where the bacteria are protected from both the innate and adaptive immunity and persist in a compartment competent for vector transmission.” Intruders below the Radar: Molecular Pathogenesis of Bartonella spp.
Bartonella Suppresses the Immune System
Another mechanism Bartonella uses to ensure its survival in humans is by suppressing the immune system response. A class of chemical compounds secreted by the immune system, called cytokines, influences the immune response. Bartonella stimulates the cytokine interleukin-10 (IL-10), which is an essential regulator of the immune system response.
When IL-10 is present, the function of immune cells is suppressed, interfering with innate and adaptive immunity. The result is a lower level of inflammation that minimizes tissue damage and symptoms. However, immune suppression by IL-10 allows Bartonella to persist in the infected person.
Bartonella Testing
A significant obstacle in diagnosing Bartonella as the cause of symptoms or illnesses is the reduced sensitivity of laboratory tests identifying the infection. For years I would rely on a clinical diagnosis of Bartonella because the laboratory testing was lacking. In recent years Bartonella testing has improved, helping clinicians know if more than Lyme disease is present.
Tests that detect antibodies against bacteria (called serology) require the immune system to see the bacteria. Bartonella primarily resides inside human cells to evade the immune system making it difficult for the immune system to mount an antibody response. Additionally, antibodies indicate exposure to Bartonella but make it difficult to confirm an active infection.
Bartonella immunoblot testing has improved upon the sensitivity and specificity of traditional antibody tests. Igenex offers a Bartonella immunoblot test that identifies four species of Bartonella. Their internal study of Bartonella immunoblot testing resulted in high sensitivity and specificity.
Another methodology for detecting bacteria in humans is to look for the bacteria’s DNA by polymerase chain reaction (PCR). PCR testing is specific to the bacteria and, if detected, indicates an active infection. The challenge of using PCR testing for Bartonella is very few bacteria circulate in the bloodstream (the bacteria are inside cells). Galaxy Diagnostics has developed a technique to increase the number of bacteria from a blood draw by growing the bacteria on an enrichment medium. Once the bacteria reach sufficient levels, the laboratory can perform PCR testing to determine if Bartonella is present. To increase the test sensitivity, Galaxy offers the option of testing three separate blood samples taken from the patient over a week.
Is Bartonella More Clinically Significant than Lyme Disease?
The number of universal vectors, including fleas, ticks, lice, and mosquitoes, that transmit Bartonella suggests Bartonellosis may be a more significant global health concern than is currently recognized. Most physicians are entirely unaware of Bartonellosis or its symptoms. Like Lyme disease, Bartonella can produce a range of symptoms, primarily neurological and psychological symptoms. Many people with Bartonellosis end up seeing specialists such as neurologists, rheumatologists, and psychiatrists, so get diagnosed with conditions that do not identify this underlying cause.
The severity of Bartonella’s disease manifestation depends upon the infected person’s immune response. Due to Bartonella’s ability to go undetected by the immune system, testing through traditional laboratories is inaccurate and should be performed by the specialty laboratories Igenex or Galaxy Diagnostics. Increasing the awareness of Bartonella vectors, symptoms, and testing will help to reduce the needless suffering for those with Bartonellosis.