We have just passed the first anniversary of the COVID-19 pandemic. No one could have predicted the life-altering impact the virus would have on every person worldwide. With the development of the COVID-19 vaccine, a decline in cases and deaths from the SARS-CoV-2 virus, the future looks bright. However, many people who were infected with the COVID-19 virus have continued to have symptoms months after the initial infection.

Late last spring, a few months into the pandemic, people with persistent symptoms following COVID-19 infection became known as Longhaulers. Since that time, health agencies have acknowledged this condition and realize it will likely affect millions of people so have given it a formal name. The National Institute of Health (NIH) refers to this condition as Post-Acute Sequelae of SARS-CoV-2 infection (PASC). The World Health Organization (WHO) uses the terminology Long COVID to describe the chronic disease that develops following infection with the SARS-CoV-2 virus. Long COVID is also the patient-preferred name.
How Many People Will Develop Long COVID?
Now that we are a year into the COVID pandemic, more research is coming out to help us understand how many people are being affected by Long COVID. In general, Long COVID is considered as a diagnosis when symptoms have persisted for 90 days or more following infection with COVID-19.
In October 2020, Kings College in London published a report tracking over 4 million people with COVID-19. They found that about 10% of people infected with COVID-19 went on to have symptoms months after the onset of their infection. In November 2020, a smaller study found that more than half of the people that were infected with COVID-19 experienced fatigue ten weeks after their initial symptoms.
In January 2021, the prestigious medical journal The Lancet published the largest study on Long COVID. The researchers evaluated 1700 people hospitalized from COVID-19 and discovered that 76% experienced at least one symptom six months after hospitalization. Fatigue and muscle weakness was experienced by 63% of the participants of the study.
The most recent study (which is still in pre-print) reviewed the medical records of over 1400 people in the University of California healthcare system. More than two months after infection with COVID, 27% of people still suffered from symptoms. What was more astounding was about a third of the study participants did not experience any symptoms when they initially tested positive for COVID. Some believe that those who did not get as sick during the acute phase might be at an increased risk of developing Long COVID because the immune system did not effectively shut down the virus.
Some people who did not have acute symptoms will go on to develop Long COVID.
Based on all the evidence available, 10%-35% of people who contract COVID-19 will go on to develop Long COVID. All age groups are affected, including children, and there is a higher incidence of Long COVID in women. The total number of cases of COVID-19 in the United States has surpassed 30 million with a half million deaths. This means to about 2.9 million to 10.3 million people (and growing) in the U.S. will end up with chronic symptoms following infection with COVID-19.
What are the Symptoms of Long COVID?
People with Long COVID have reported over 200 symptoms. A comprehensive list of symptoms from an international study can be found here. The more common symptoms are:
- Fatigue
- Brain fog
- Shortness of Breath
- Chest pain/tightness
- Palpitations
- Cough
- Fever
- Abdominal pain
- Anxiety
- Low back pain
- Muscle aches and weakness
- Insomnia
- Diarrhea
- Change in the sense of smell and taste
- Dizziness/lightheadedness
Other Conditions Associated with Long COVID
- Autoimmune disease
- Dysautonomia/POTS
- Mast cell activation syndrome
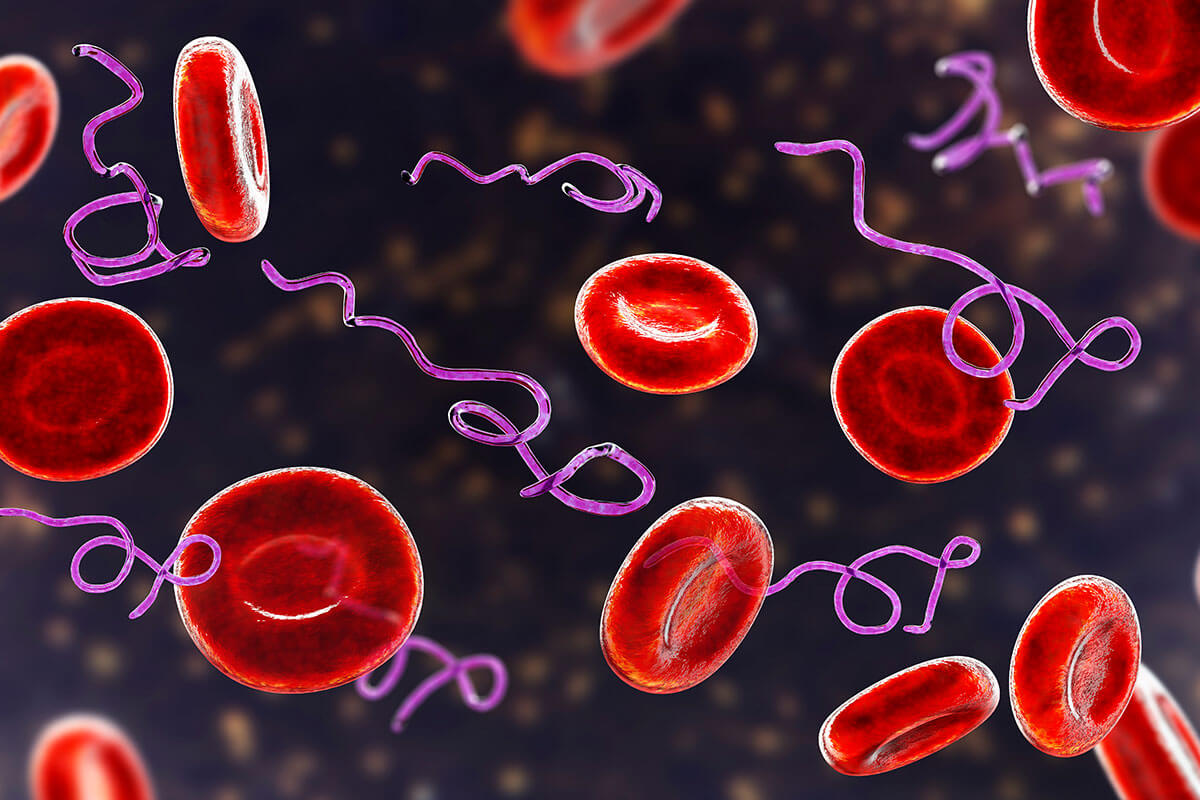
- Tickborne infections (Lyme disease, Bartonella)
- Mycoplasma bacteria
Is Long COVID an Autoimmune Disease?
One cause of autoimmune reactions in the human body is through a mechanism called molecular mimicry. Molecular mimicry (also known as cross-reactivity) occurs when a pathogen has a similar protein sequence to human tissue. The consequence is antibodies made to attack a pathogen also attack human tissue (joints, thyroid, etc.).
In January 2021, researchers from southern California published their findings of a study to determine if SARS-CoV-2 virus antibodies could cause an autoimmune reaction. They tested human monoclonal SARS-CoV-2 antibodies against 55 human tissues. What they discovered was remarkable – COVID-19 antibodies cross-reacted with a total of 28 human tissues!
COVID-19 antibodies cross-react with mitochondria which may be the cause of chronic fatigue in Long COVID
The most common human tissue the antibodies reacted to was the energy-producing powerhouse, the mitochondria. If COVID-19 antibodies are also destroying human mitochondria, it makes sense a common symptom of Long COVID is fatigue. Other tissues that COVID antibodies cross-reacted with were gastrointestinal, thyroid, muscle, and brain. Other studies have reported autoimmune thyroiditis following infection with COVID-19.
Does the COVID Vaccine Contribute to Autoimmune Disease?
The authors from the above study set out to answer another question: if antibodies to COVID-19 attack normal human tissue, will the COVID vaccine contribute to autoimmune disease? Vaccines work by triggering the immune system to form antibodies against a pathogen. The results of this research project confirmed cross-reactivity between SARS-CoV-2 antibodies and human tissues. At this time, we do not have long-term data to conclude if the COVID vaccine will increase the incidence of autoimmune diseases.
Mitochondrial Function in Energy and Immunity
Mitochondria are organelles in every cell of the human body and produce 90%-95% of the body’s total energy. Highly metabolic tissues such as the heart, brain, and muscles have the highest concentration of mitochondria in each cell. Mitochondria are damaged by oxidative stress from toxins, infections, and other insults.
When the mitochondria do not function properly, the primary energy compound (ATP) is not produced in sufficient quantities and metabolic function slows down. The immune system requires normal-functioning mitochondria. If a virus damages mitochondria, the immune system that is needed to knock out the virus becomes compromised.
Is Long COVID a Result of Mitochondrial Dysfunction?
Mitochondrial dysfunction has been associated with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Viral infections, including Epstein-Barr Virus (EBV) and Human Herpes Virus 6 (HHV-6), have been implicated as a cause of ME/CFS, possibly due to mitochondrial dysfunction. The authors of a paper published November 2020 suggest treatments that support mitochondrial function and have proven effective in ME/CFS may also be effective for Long COVID.
Part of the treatment strategy I have taken with patients suffering from Long COVID is supporting mitochondrial function. I have found intravenous NAD with nutrient co-factors effective at restoring mitochondrial function. I know of at least one research study currently underway looking at the effectiveness of NAD for fatigue associated with Long COVID.
Not Repeating Mistakes Made in Chronic Lyme Disease and ME/CFS
Acute infection with the SARS-CoV-2 virus causes symptoms similar to other infections that develop into chronic conditions. John Hopkins University physician John Aucott, MD, published a case report of a delayed diagnosis of Lyme disease in a patient who was thought to have COVID-19.
Early in the pandemic, the Lyme disease and ME/CFS communities observed similarities in Long COVID that they had faced for years – testing was inadequate, treatments were ineffective, and healthcare providers did not believe them. On March 5, 2021, a correspondence written by Dr. Aucott was published in The Lancet cautioning the healthcare community to not make the same mistakes with Long COVID that were made with Lyme disease and ME/CFS.
“Although the frequency, severity, and potentially the etiology of persistent symptoms can vary, sequelae after COVID-19 appears poised to join the range of other postinfectious syndromes described in the field of infectious diseases. These often share a common symptom phenotype, which might also meet case definitions for myalgic encephalomyelitis/chronic fatigue syndrome, fibromyalgia, or post-treatment Lyme disease. We hope that researchers and clinicians will draw on these other conditions as they continue to advance scientific understanding of so-called long-haul or persistent COVID-19. We would also argue that there are important lessons to learn and pitfalls to avoid; our specific area of clinical care and research (post-treatment Lyme disease) has remained a fiercely contentious condition for more than 30 years.”
Congress recently passed a COVID relief bill that earmarked over $1 billion for Long COVID research. The research findings may also benefit the underfunded Lyme disease and ME/CFS communities since there may be similar dysfunction amongst these illnesses.
Do Pre-existing Infections Contribute to Long COVID?
It has been reported infections including Bartonella and Mycoplasma can become reactivated during an infection with COVID-19. People who develop persistent symptoms (Long COVID) following infection with the SARS-CoV-2 virus may have had underlying low-grade infections reactivated by the acute COVID-19 infection.
Physicians should include comprehensive testing for viral and bacterial infections, including Lyme disease, Bartonella, Mycoplasma, and Epstein-Barr Virus, in the diagnostic evaluation of Long COVID.
Molecular Fingerprint Similarities in COVID-19, ME/CFS, and Lyme Disease
A recently released study that is still in pre-print (has not been peer-reviewed) looked at molecular patterns of ME/CFS and compared the results to some chronic infections and autoimmune diseases. Blood and immune cells from the ME/CFS patients and control groups were analyzed with RNA sequencing to develop molecular signatures. The researchers developed mathematical models where they identified 904 “key driver genes” in ME/CFS.
Surprisingly, molecular patterns in ME/CFS were similar to patterns in Lyme disease and COVID-19 and not the autoimmune conditions tested. This suggests a “common underlying biology that shares immune and metabolic dysregulation.”
The findings from this complex study may explain why people that develop Long COVID may have a similar clinical path as those with ME/CFS and Lyme disease.
What Can be Done for Long COVID?
We are just beginning to see the long-term health effects that will come from this pandemic. Research studies are being published with various theories about the cause of Long COVID. Still, more time needs to pass and research conducted before we have a clear understanding of the underlying pathophysiology of Long COVID.
A handful of university hospitals have created Long COVID clinics to serve the wave of people who will become afflicted with chronic symptoms. Since there is no approved treatment for Long COVID, many of these clinics only offer symptomatic treatment and seek to collect data. Physicians with experience treating other chronic illnesses such as Lyme disease and ME/CFS are best qualified to help those who develop Long COVID.