Pain and arthritis are two of the most common symptoms of Lyme disease. Lyme disease was discovered in 1975 because of an outbreak of pain and arthritis in children and adults in Lyme, CT. After calls to the CDC by concerned parents, rheumatologist Alan Steere was sent to Lyme to investigate this bizarre cluster of symptomatic people. Originally thought to be a rheumatological disease, it was not until a few years later the cause of the pain was identified as an infection with the bacteria Borrelia burgdorferi.

Arthritis caused by Lyme disease occurs after the bacteria from a tick bite has spread to joints. It may take months to years following a tick bite before pain manifests, so Lyme disease as the cause of pain may be overlooked. In 60% of people with arthritis caused by Lyme disease, it can take up to 2 years after someone has been infected for the diagnosis to be made. In children with Lyme disease presenting with pain, 20% are misdiagnosed at initial evaluation.
What Does Pain in Lyme Disease Look Like?
Arthritis can present in one joint (monoarticular), 1-3 joints (oligoarticular) or multiple joints (polyarthritis). In children, pain most often occurs in 1-3 joints. Pain in multiple joints is also involved in the autoimmune conditions lupus and rheumatoid arthritis. This can make it challenging to obtain a correct diagnosis if Lyme disease is the underlying cause. Because the bacteria spread throughout the body, any joint can be affected.
Larger joints such as knees, hips, and shoulders are most common joints affected in Lyme disease.
In addition to pain in joints, Lyme disease can also cause muscle pain. This is another scenario where people often get misdiagnosed, this time with fibromyalgia. In fibromyalgia, the pain would be more dispersed, and there would be no joint inflammation.
Since fibromyalgia describes the symptomatic presentation of the pain, and there is no known cause, Lyme disease and associated infections should be considered as a cause.
The bacteria that causes Lyme disease can directly or indirectly damage nerves leading to nerve pain, numbness, and tingling. The infection sets off an inflammatory immune response leading to the destruction of the protective coating of nerves called myelin sheaths.
Pain in any location can be dull and ache or be sharp and shooting. It is common for pain in Lyme arthritis to migrate from one joint to another, so one day pain may be in a knee and in the neck the following day. Another unique presentation is Lyme bacteria have an affinity for previously damaged tissue, possibly because that tissue is already inflamed and has a poor immune response. An old knee or hip injury that becomes chronically painful and is often attributed to the old injury. Additionally, there may be a cyclical pattern to pain caused by Lyme disease due to bacteria fluctuating between dormancy and being active.
It is rare to see migrating pain and a cyclical pattern to pain in other forms of arthritis.
In addition to the pain caused by Lyme disease, a person will often experience accompanying symptoms such as fatigue, headaches, fevers and brain fog that are not seen with other causes of pain.
How Does Lyme Disease Cause Pain?
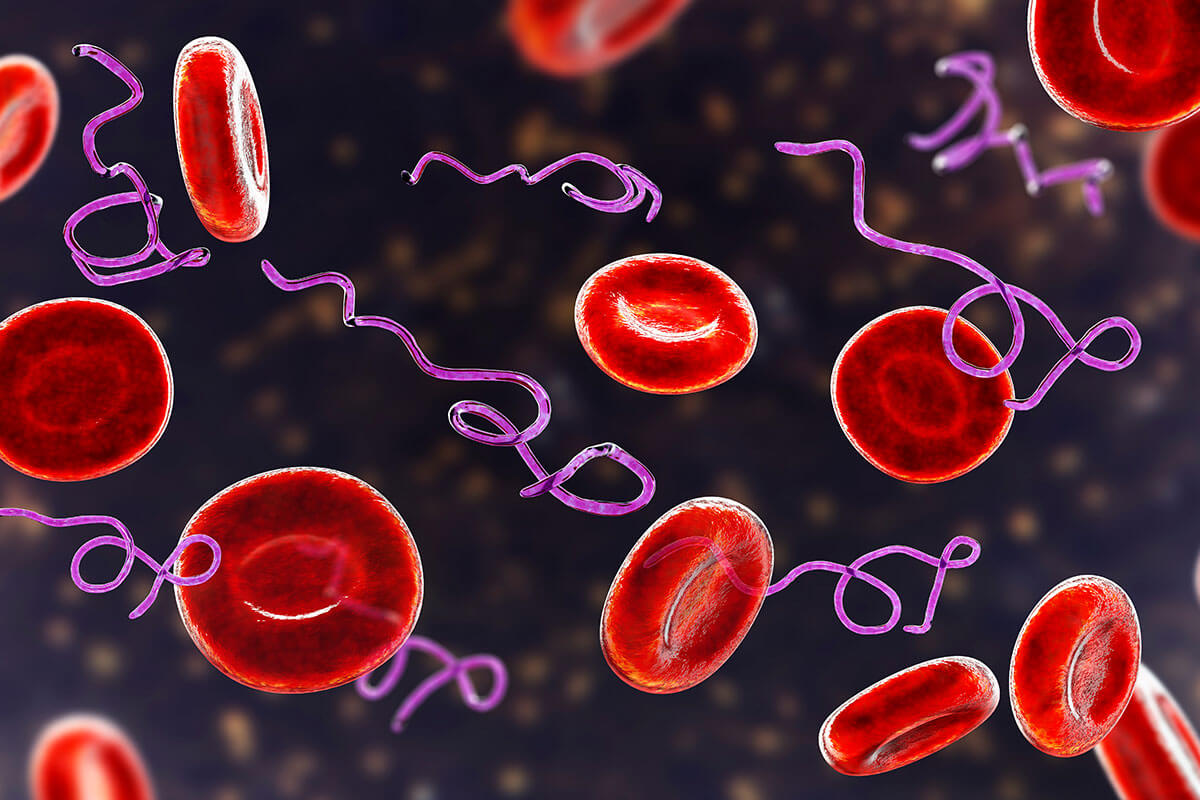
The presence of Lyme bacteria triggers a physiological cascade that leads to pain and inflammation.
First, the bacteria travel to joints and connective tissue where they cause direct damage to that tissue. Then the immune system releases cytokines in response to the infection, which in turn creates inflammation. The bacteria can also trigger an autoimmune reaction where the antibodies that are made in response to the bacteria begin to attack the body’s tissue.
This autoimmune concept is known as molecular mimicry and can lead to conditions such as rheumatoid arthritis and lupus. Ultimately the goal is to find and treat the cause of the symptoms or diagnosis.
In late-stage Lyme disease, it can be challenging to determine if the infection is still causing symptoms or if the bacterial load has decreased, but the immune response persists creating inflammation. This is a central debate in chronic Lyme disease, and some have termed the latter symptoms Post-treatment Lyme Disease (PTLD). My approach is to treat both the infection and the overactive immune response.
Damon is an 8-year-old boy who presented to the local hospital’s emergency department because of a very swollen and painful knee. The hospital referred him to the children’s hospital so he could be cared for by pediatric rheumatologists and orthopedists.
The doctors at the children’s hospital performed an aspirate of the fluid in Damon’s knee. His parents requested the fluid be tested for the bacteria that causes Lyme disease since Damon had a history of Lyme disease. The doctors were reluctant because Lyme disease is rarely considered as a diagnosis in California. To the doctors’ surprise, the fluid from Damon’s knee was positive for Lyme disease.
Damon’s parents brought him to my office later that week. I ordered a full tick-borne infection panel that was not only positive for Lyme disease but also Bartonella – another tick-borne infection. I prescribed Damon herbal tinctures for Lyme and Bartonella, and within a week, the swelling had reduced significantly, and within a couple of months, the pain had resolved.
Diagnosis of Lyme Arthritis
Like all proper diagnostic workups, it is essential to start with the history of the patient. In the case of tick-borne infections, it is important to know if there is a possibility the person may have been exposed to a tick prior to the onset of their symptoms. As mentioned previously, it can take up to two years for the pain caused by Lyme disease to manifest, so it is essential to review the patient’s history. Does the person spend time outdoors? Some activities increase exposure risks such as hiking, horseback riding, and camping, but people can also be exposed to ticks in parks, sports fields, in their yards, and from their pets bringing ticks into the house.
When children experience pain, they are often taken to their pediatrician who may not consider the diagnosis of Lyme disease. The same can occur for an adult with pain who presents to an orthopedist or sports medicine doctor.
On exam, the lining of the affected joint may be inflamed – called synovitis. Synovitis not only occurs in rheumatoid arthritis but also Lyme arthritis. Lyme arthritis rarely causes symmetrical joint involvement like rheumatoid arthritis, which can be helpful in making the correct diagnosis.
Lab Tests to Determine the Cause of Arthritis
If a tick-borne infection such as Lyme disease is a possible cause of pain, a comprehensive tick-borne infection panel at a Lyme-specific specialty laboratory should be ordered. Traditional rheumatology tests will provide insight into the underlying cause of pain and arthritis.
A positive low-level ANA (anti-nuclear antibody) is not specific to lupus or rheumatoid arthritis and can also be elevated in Lyme disease. Anti-CCP antibodies are specific to rheumatoid arthritis and rarely positive in Lyme arthritis, so are helpful in distinguishing Lyme arthritis from rheumatoid arthritis.
An erythrocyte sedimentation rate (ESR) can demonstrate the degree of inflammation in the body, but is only significant above 50 mm/hr. The test creatinine phosphokinase (CPK) tests for inflammation in the muscles, called myositis. Myositis is rare in children, except in Lyme disease and polymyositis, so CPK may be a useful test.
Synovial fluid from the affected joint can provide valuable information. In Lyme arthritis, the fluid will be yellow, have thin viscosity, be cloudy or turbid, and have a white blood count from 5,000-50,000. The white blood count in septic arthritis will be much higher. Lyme tests like PCR can be performed on synovial fluid.
Imaging for Lyme Arthritis
X-rays are a helpful diagnostic tool to identify the cause of arthritis and pain. Joint space narrowing is the hallmark finding on X-ray in osteoarthritis, and not seen in other causes of joint pain. Lyme disease rarely causes changes of the bones on X-ray.
Soft tissue swelling will be seen with Lyme disease and trauma, not in other conditions.
An MRI of a joint is useful at differentiating Lyme arthritis from septic arthritis or structural damage. In Lyme disease, an MRI will demonstrate joint effusion, synovitis, and muscle edema (myositis).
Treating Pain Causes by Lyme Disease
When Lyme disease is the cause of pain and arthritis, the primary goal is to remove the bacteria that started a cascade of reactions that contributed to the pain. Just as importantly, the fire of inflammation that has been lit needs to be treated. This inflammation is present with active infections, but can also persist after the infections are successfully treated.
Diet
The foundation for reducing systemic inflammation in the body is to avoid foods that are inflammatory. The foods that most commonly create inflammation (even if there is no allergy to them) are gluten, cow dairy, and sugar. If food allergy testing has been performed, the reactive foods should also be avoided. People with other conditions such as SIBO (small intestinal bacterial overgrowth) or MCAS (mast cell activation syndrome) may also need to follow a specific diet. Any food that creates inflammation adds to the level of inflammation already being produced by infections.
Herbal Treatment for Pain
The herb turmeric is one of the most effective treatments for reducing the pro-inflammatory cytokines produced by the immune system in response to tick-borne infections. This reduction in inflammation leads to a reduction in muscle and joint pain, and joint swelling.
A therapeutic dose of turmeric is needed, so cooking with this spice alone will not accomplish the pain-relieving effects. Turmeric is poorly absorbed, so a high-quality turmeric with good absorbability should be taken. Since turmeric is safe and natural – and has many other benefits besides reducing inflammation – it should be considered as a therapy for anyone suffering from pain.
Low-dose immunotherapy (LDI)is a promising therapy that works to improve the immune response in Lyme disease
LDI uses very dilute doses of bacterial antigens to help down-regulate the inflammation produced by bacteria. This treatment has provided remarkable benefits for many people who suffer from pain and neuropathy from Lyme disease and associated infections.
Not to be confused with low-dose immunotherapy (LDI), low-dose naltrexone (LDN) is another effective therapy for reducing pain and inflammation induced by Lyme disease
Naltrexone is manufactured at a dose of 50mg for alcohol and drug addiction, but when used at much smaller doses, it has a broad range of applications including treatment of autoimmune conditions and pain reduction. Like LDI, the most effective dose of LDN is unique to each person so a trial of the medication with a range of dosages is essential. Patients can start as low as 0.5mg and increase up to 4.5mg, staying on each dose for a week. Keeping notes of symptoms at each dose helps to identify the most effective dosage. Note, LDN works by blocking opiate receptors, so LDN is contraindicated while on opioid-based pain medication.
Ten-pass ozone therapy helps reduce pain and inflammation associated with Lyme disease and tickborne infections
Introducing ozone to a quantity of blood – also known as major autologous hemotherapy (MAH) – has been safely used around the world for decades. In MAH, blood is removed from the patient and mixed with ozone in an IV bag, then infused back into the patient. Ten-pass ozone is a closed system so ozone can be administered in a hyperbaric state for multiple “passes.” This creates a much higher dose of ozone than traditional MAH, and is more effective at reducing pain and inflammation.
There are other natural therapies such as glutathione and alpha lipoic acid that can be effective at reducing pain and inflammation. Over-the-counter and prescription medications such as NSAIDs and anti-rheumatic drugs can reduce pain, but can come with a cost so are best to avoid.
Practical Assessment and Treatment of Pain, Arthritis, and Fibromyalgia in Lyme Disease
Pain is common in early and late-stage Lyme disease. The first, and most important, step is proper testing to determine if Lyme disease and/or associated infections are the cause of the pain. Bacteria from tickborne infections can directly damage joints, trigger an immune response that creates inflammation, and cause an autoimmune reaction that leads to pain.
If symptoms such as fatigue, headaches, fevers, or brain fog are present along with pain, this suggests a systemic infection may be involved. Infections can trigger autoimmune conditions such as rheumatoid arthritis and lupus, so a thorough investigation is warranted. Multiple therapies can help reduce pain and inflammation caused by Lyme disease and associated infections, but ultimately successful treatment of the infections is most important.