When individuals are afflicted with chronic illnesses, their cellular structures are not immune to collateral damage. Chronic infections, environmental toxins, and other sources of inflammation and oxidative damage can harm cell membranes and inner cellular structures like mitochondria, impacting cellular structure and function. It’s crucial to understand that the cause or causes of the illness can be effectively treated, yet symptoms may persist due to lingering cellular damage. This emphasizes the importance of understanding cellular health. Lipid replacement therapy, particularly with phosphatidyl choline, has emerged as a potential solution, improving cellular health and recovery from chronic illnesses.
The Role of Cell Membranes
It is estimated that humans have about 50 trillion cells in their bodies. Each cell has an outer membrane of lipids that allows nutrients into cells and waste products from metabolism to leave cells and serves as a protective barrier. In addition, receptors in the cell membrane transmit hormones and neurotransmitters into cells. Inside cells, membranes create compartments that allow biochemical reactions to occur. Essentially, cell membranes create a structure for the cell, allowing it to perform its essential tasks and protecting the intracellular content from external damage.
Mitochondria Produce Energy
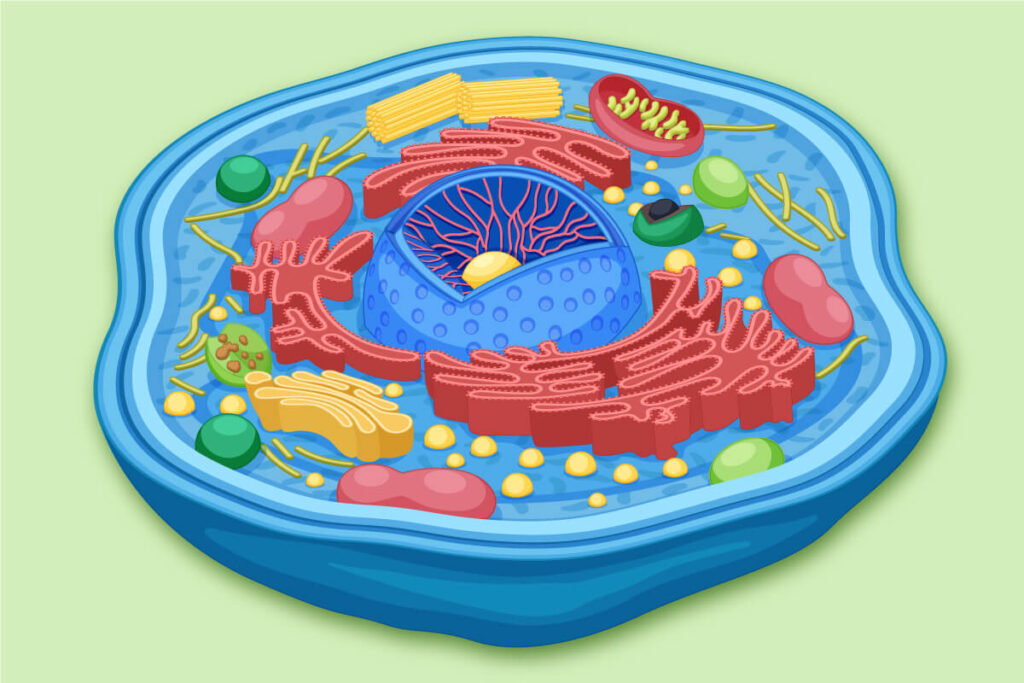
Within our cells are specialized structures called organelles. Mitochondria, one of the most crucial organelles, produce up to 95% of the body’s energy. They produce ATP, the energy currency of our cells, which cannot be stored and thus requires efficient mitochondrial function for continuous production.
Remarkably, the human body produces more than its body weight in ATP daily, a testament to our cells’ incredible energy production capabilities
On average, there are 1000-2000 mitochondria per cell. Organs with higher energy demands, such as the brain, heart, and immune system, can have up to 2 million mitochondria per cell. With 50 trillion cells and 1000-2000 mitochondria per cell, it’s easy to see the critical role mitochondria play in proper metabolism. Cellular metabolism slows, and energy production is reduced when mitochondria are damaged or a threat from an infection or toxin is sensed. A model that describes this concept is the cell danger response, a protective mechanism that slows down cellular metabolism and energy production when the cell senses a threat, such as an infection or toxin, to prevent further damage.
The Role of Mitochondria in the Immune Response
Cellular metabolism and immune function are not separate entities but tightly interconnected. The field of study linking immune cells and mitochondrial function is known as immunometabolism.1 The mitochondria play a critical role in immune cells’ growth and function. The immune system uses 15-20% of daily energy in healthy individuals. When a person has an infection, the immune system’s energy consumption increases by 25%.2 Mitochondria structure and function changes affect lymphocyte function, increasing inflammatory cytokine production.3 This interconnectedness is a crucial aspect of immune health.
Cell Membrane Damage
Cell membranes function best when they are fluid and flexible. When cell and mitochondrial membranes are damaged, they become stiff and rigid, interfering with their ability to perform their functions properly. Physical trauma, exposure to heavy metals, mold toxins, and bacterial and viral infections damage cellular, mitochondrial, and DNA membranes. Aging is also associated with cellular membrane changes and lipid imbalances. If membranes are damaged and not repaired, it can lead to inflammation, tissue dysfunction, disease, and cancer. The laboratory marker malondialdehyde (MDA) reflects the level of lipid oxidative damage.4 Elevated MDA can elicit an immune response similar to the immune response to an infection or toxin.
Causes of Mitochondrial Damage
- Aging and oxidative damage
- Toxic metals – lead5, mercury6, arsenic7
- Infections – viral and bacterial
- Mold and mycotoxins8
- Industrial and agricultural toxins9
- Prescription drugs – Tylenol, aspirin, anti-depressants, L-dopa, NSAIDS, statins, valproic acid, fluoroquinolones, and some chemotherapy drugs10
- Alcohol11
DNA Adducts in Chronic Disease
DNA adducts form when chemical compounds bind to DNA gene regions. Genes create instructions that influence characteristics and function in the body. Adducts affect gene transcription, interfering with the expected message produced by a gene region. Adducts can form on mitochondrial DNA. Adduct formation results from exposure to various chemicals, carcinogens, and other toxic substances. Cells have their DNA repair mechanism, and DNA adducts can interfere with their ability to correct DNA damage. Ultimately, DNA adducts lead to cell damage and dysfunction. DNA adducts can be measured and effectively treated to improve cellular function.
Phosphatidyl Choline is Abundant in Cell and Mitochondrial Membranes
It is clear that cellular and mitochondrial membrane health is essential for optimal cell function, and damaged cell membranes play a pivotal role in the persistence of symptoms in chronic illnesses. Inside mitochondria is another critical membrane called cardiolipin, where energy production occurs.12 Cardiolipin membranes are delicate and susceptible to oxidative damage.13
If cellular and mitochondrial membranes are damaged from exposure to toxins, infections, and other causes of oxidative damage, how can the membranes be repaired? Phosphatidyl choline is the most abundant phospholipid in cell and mitochondrial membranes.14 Research studies have shown that mitochondrial dynamics and functions are significantly impacted when a modest amount of mitochondrial phospholipid is reduced.15
Conditions That May Benefit From Lipid Replacement Therapy
- Mold-related illness16
- Lyme disease and other chronic infections17
- Long COVID 18
- Chronic fatigue syndrome19
- Multiple sclerosis20
- Parkinson’s disease21
- Dementia22
- Neuropathy23
Phosphatidyl Choline Supports Detoxification
Environmental toxins directly damage cell membranes, interfering with their ability to efficiently move nutrients into cells and waste products out of cells. Toxins can also become incorporated into cell membranes, affecting their ability to function. An increased toxic burden in cell membranes contributes to the collateral damage and persistent symptoms people experience in chronic diseases. Phospholipids replacement therapy can aid the body in detoxifying toxins from membranes and repairing the damage induced by toxins.
Why Does Chronic Disease Persist?
When someone has a chronic illness or has been treated for a chronic infection or toxic burden but still has symptoms, their cells have been exposed to oxidative stress. The underlying cause (or causes) of the symptoms may have been successfully treated, but the symptoms persist due to damage on a cellular level. In my practice, I commonly see this contribute to symptoms and cause illnesses to persist.
“Chronic disease persists because healing is incomplete” Robert Naviaux, M.D.
Lab Testing for Cellular and Mitochondrial Health
Cell and mitochondrial membrane health is measured through laboratory testing to determine its role in chronic disease and symptoms. The inner mitochondrial membrane, cardiolipin, can be measured to assess mitochondrial health. Cell membrane phosphatidyl choline can be analyzed and, if low, indicates the need for phosphatidyl choline administration. The marker of cell membrane damage, malondialdehyde (MDA), signifies the severity of oxidative damage to cell membranes. Laboratory testing can also determine if DNA adducts are present.
You Are Only as Healthy as the Health of Your Cells
With over 50 trillion cells and significantly more mitochondria, cell and mitochondria membrane health plays a crucial role in our overall health. I often share with patients that their cells make up tissues, tissues make up organs, and organs make up humans. Many people with chronic diseases, autoimmune conditions, and persistent symptoms, including fatigue, remain ill due to oxidative damage to cellular structures. This impedes proper cell and mitochondrial function. Taking nutrients that support mitochondrial function without repairing cellular structures is ineffective.
We live in a time challenged with chronic illness. Functional medicine has opened minds to the concept of root cause medicine, but as we traverse through the body’s systems; hormones, gut health, etc, we understand just how intricately the body is connected. So what if we focused on the genesis of all living things – the cell. If our cells can be repaired then we conquer all illness! Krishna Doniparthi, MD
Specialized laboratory testing can quantify cellular health and provide a roadmap to healing complex chronic illnesses. Research has demonstrated that administering 0.5-1.2 grams of intravenous phosphatidyl choline per kilogram of body weight repairs damaged cell membranes, clears DNA adducts, and improves patients’ health. I have observed patients’ health improve and laboratory results normalize after completing a comprehensive treatment protocol. This approach provides a roadmap and hope to help those suffering from persistent symptoms related to complex chronic illnesses.